Habibat Ohunene Lawal and Dr Adachi Ekeh (Lead writers)
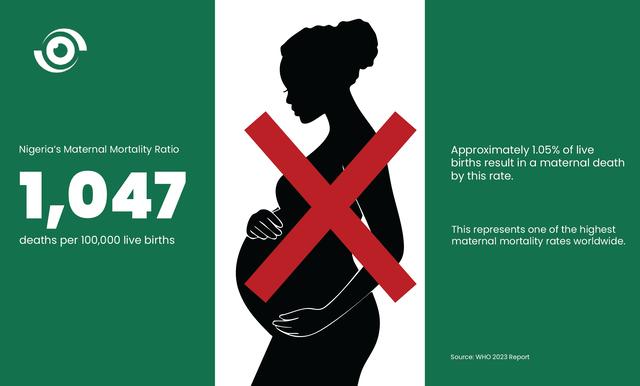
Postpartum haemorrhage (PPH), prolonged bleeding after childbirth, remains the leading cause of maternal mortality, accounting for 23% of maternal deaths. In 2023, the World Health Organisation (WHO) estimated Nigeria’s maternal mortality ratio to be 1,047 deaths per 100,000 live births, the world’s second-highest.
The statistics tell a stark story. More than 80% of these deaths occur in sub-Saharan Africa and South Asian countries, where the fragile health infrastructure, unavailability of care, and the endemic problem of substandard drugs turn a largely preventable complication into a leading killer of women.
Uterotonics, including oxytocin, misoprostol and carbetocin, are the frontline medicines recommended by WHO to prevent PPH. They work by stimulating uterine contractions immediately after childbirth, contracting the uterus and tightening blood vessels to reduce bleeding. These medicines have become standard of care in preventing and managing PPH. Yet, an insidious epidemic of substandard and falsified oxytocin, one of the most widely used uterotonics, is undermining this lifesaving intervention.
This crisis is compounded by poor storage and weak cold-chain systems. Because oxytocin is temperature-sensitive, it must be stored at 2°C to 8°C to maintain its potency. Without refrigeration, the drug degrades into an inactive liquid, offering patients and healthcare providers only a dangerous illusion of safety.
One proven, step-by-step approach to managing PPH is the E-MOTIVE bundle which depends on the effectiveness of each component, including oxytocin. However, the success of this treatment can be compromised if oxytocin is of poor quality.
The hidden costs of poor-quality Oxytocin
In Nigeria, a 2021 survey found that only 46% healthcare workers knew that oxytocin should be stored in a refrigerator; just 34% reported that their facilities stored oxytocin in a refrigerator; and an alarming 74.2% of oxytocin samples failed quality tests.
When oxytocin fails, the result is a health emergency that places enormous strain on already fragile systems, depleting blood banks, occupying scarce operating rooms, and diverting skilled staff. The ripple effect is clear, every preventable case of postpartum haemorrhage pulls critical resources away from other essential maternal and child health services.
In rural primary health centres (PHCs), where blood transfusion services are not part of the minimum service package, a mother experiencing severe bleeding must be referred to a higher-level facility. But what if she cannot afford the cost, has no transport, or the nearest hospital is too far away?
In such situations, public confidence in the health system erodes, discouraging mothers from seeking care. Fearing hospital interventions will fail, some choose home births instead, placing themselves at greater risk of PPH and perpetuating poor maternal health outcomes.
Finally, the emotional toll on health workers is immense, contributing to healthcare worker burnout and high turnover. Witnessing avoidable deaths, despite following protocols, leaves them demoralised and undermines the system’s ability to deliver.
The price of substandard Oxytocin
The widespread use of poor-quality oxytocin creates a devastating economic burden that extends far beyond drug itself. It drives up healthcare expenditure, erodes public trust, and results in a long-term loss of human capital and economic productivity.
When oxytocin fails, early signs of PPH can rapidly escalate into a medical emergency that triggers a series of costly interventions. Emergency blood transfusions, which are expensive to acquire, screen, and deliver, are often the first recourse. Many patients then require extended stays in intensive care units (ICUs), where the average deposit is around ₦500,000 (approximately US$330), a sum far beyond the reach of most Nigerians earning the current minimum wage of ₦70,000 (US$ 47).
These costs are rarely covered by health insurance, forcing families to rely on out-of-pocket payments that push the most vulnerable into financial ruin. The failure of the drug also drives up surgical costs, as women may need emergency hysterectomies. Ironically, it even inflates drug expenditures. Physicians often administer multiple doses of the ineffective oxytocin before moving to more expensive second-line medications.
These economic shocks show clearly Nigeria’s wider health financing challenge, where out-of-pocket spending dominates and underfunded insurance schemes leave families without a safety net.
Beyond the drug: building systems that save lives
The Smiles for Mothers project represents a bold, targeted response to Nigeria’s maternal health crisis. Led by Solina Center for International Development and Research (SCIDaR) in partnership with the Clinton Health Access Initiative (CHAI) and Health Strategy and Delivery Foundation(HSDF) it is addressing PPH by implementing WHO guidelines and introducing a heat-stable carbetocin, a breakthrough drug that does not require cold-chain storage and brings life-saving innovation to low resource settings.
What makes this effort powerful is its human centered design. Beyond introducing a new drug, it strengthens fragile supply chain, equips health workers to recognise and report counterfeit or substandard medicines, and reinforces regulatory reporting systems. These steps build trust, awareness, and demand for safe maternal care.
The true cost of substandard oxytocin is measured not only in the lives of mothers lost, but in avoidable healthcare spending and the long-lasting social and economic scars left on families and communities. Ultimately, success will be measured in lives saved, by ensuring that every woman, regardless of where she gives birth, can rely on the quality and integrity of the medicines meant to protect her.