(1) Why are vaccines important in the COVID-19 pandemic?
The COVID-19 outbreak has evolved into a historic pandemic, bringing unprecedented disruption to global economies. In response to the outbreak, public health measures including handwashing with soap and water, physically distancing and wearing of face masks have been recommended to limit transmission. The pandemic has caused a great deal of disruption and anxiety, and people are eager to get back to their normal lives. However, we cannot wish the virus away, and it will not disappear on its own. So, our best bet out of the COVID-19 pandemic is through a vaccine, as long as it provides full protection against SARS-CoV-2, the virus that causes COVID-19. Vaccines are one of the most impactful healthcare interventions and have contributed to a decrease in many infectious diseases and saved millions of lives.
Despite the benefit of all the recommended public health measures in preventing transmission, vaccines still provide us with the best chance of our lives returning to some semblance of normality. However, the development of a vaccine will not lead to the immediate end of the pandemic, and will not be a “silver bullet”. People must not abandon the public health measures recommended by national public health institutes. Our best bet right now, is still prevention by adhering to the public health measures, detection through testing, isolation and treatment when ill.

(2) What must an effective vaccine have?
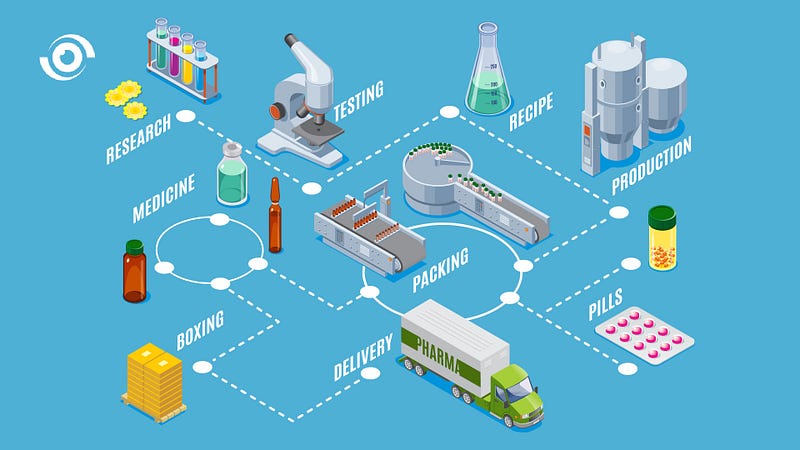
Many vaccines are currently in development and at various stages of clinical trials. In the past, it has generally taken over 10 years to develop a vaccine. However, given the advancement in science, and funding streams available, the development of a COVID-19 vaccine has been accelerated more than ever before. Despite the fast tracking of many activities, vaccines must be safe, effective, well tolerated, preferably long lasting and protect people from the getting the COVID-19 viral infection (or at least disease). In the development of an eventual vaccine, there can be no compromise on safety and trials must follow all safety protocols in phase 1 and 2, with even more intensified adherence to in phase 3 trials where the key objective is to test for protection against COVID-19. Even after all the phases of clinical trials, long-term follow up is necessary to ensure long-term safety, making the need for surveillance systems for adverse events relating to vaccines more important than ever before.
(3) What COVID-19 vaccines are closest to licensure?
Currently there are several COVID-19 vaccines under development and at various stages of clinical trials. The announcement of the Pfizer and BioNTech vaccine, which is reported to have a 90% effectiveness in preventing COVID-19, is an encouraging development. Early results have also been reported from trials of a COVID vaccine developed in Russia, suggesting it could be 92% effective. We await the publication of more details from both reports to understand if the measure of effectiveness reported is against the virus or the disease. The vaccines’ reported efficacy exceeds the Food and Drug Administration (FDA) requirement for a vaccine to have an efficacy of at least 50% against COVID-19. However, it is important to note that there are other vaccines in the pipeline and it is likely that we will end up with a number of vaccines with different effectiveness profiles.
There is a lot to digest when trying to understand the different stages of vaccine development and clinical trials, with many considerations to take into account for a safe and efficacious vaccine. So, to keep track of all the current vaccines at various stage of development and clinical trials, refer to the COVID-19 Vaccine Tracker, which collates information from the WHO website for ease of access.
(4) What is COVAX?
The Access to COVID-19 Tool (ACT) Accelerator is a global collaboration by WHO and many of the major players in global health security to speed up the development, production and equitable access to COVID-19 diagnostics, therapeutics and vaccines. COVAX is the vaccine pillar of the (ACT) Accelerator which aims to ensure that over 2 billion doses of COVID-19 vaccines receive regulatory approval, by the end of 2021. They do this by supporting research and development into new vaccines and working with pharmaceutical companies to negotiate an appropriate price to improve access. The COVAX facility acts as a kind of insurance plan, providing countries that sign on, with access to a wide range of COVID-19 vaccines, and so reducing the uncertainty and risk of investing in a vaccine that does not succeed. Nigeria is one of the countries that will benefit from vaccines procured through the COVAX facility.
The COVAX facility is co-lead by the Coalition for Epidemic Preparedness and Innovation (CEPI), Gavi, the Vaccine Alliance and the World Health Organization (WHO). CEPI was started in order to carry out research and development into vaccines for diseases that have pandemic potential. Gavi, is an organisation that supports the provision of vaccines to children from low incomes countries at an affordable cost. It is responsible for coordinating and administering the COVAX facility, and also helping to build the logistics and supply chain channels for the vaccine. WHO is pushing to get commitment from its member countries to support and join the COVAX facility.
(5) Who have contributed to COVAX?
While participation was tepid initially, over 94 high income countries are now paying into the COVAX facility from their public finance budgets. These collected funds invested in specific companies with vaccine candidates will provide vaccine manufacturers with the required investments to drive development through the clinical trial phases and to production, once a vaccine is approved. By pooling funds in this way through the COVAX facility will mean that negotiated prices with manufacturers are lower, therefore benefiting lower income countries and enabling them to have access to a COVID-19 vaccine, through Gavi’s Advanced Market Commitment (AMC).

(6) Who has access to vaccines from COVAX?
COVAX will enable all countries to have access to a diversified portfolio of vaccines. In addition to low income countries that will get an agreed number of vaccine doses for free, high and middle incomes that have invested directly in COVAX, will be also be able to procure a potential vaccine for their population. What is quite encouraging about COVAX is that it is a collaboration between governments, philanthropists and non-governmental organisations. The Advanced Market Commitment (AMC) will enable the securing of COVID-19 vaccines for lower — middle income countries. This is a global pandemic and there is an urgent need to control it and to ensure that all people globally have equitable access to a vaccine. Currently, over 190 countries have signed up to the COVAX facility, representing about 90% of the global population.

(7) How can we deliver vaccines once available in Nigeria?
The National Primary Health Care Development Agency (NPHCDA) leads on Nigeria’s vaccination policy and implementation. From its work on delivering on campaigns for vaccine preventable diseases in Nigeria, including polio, it has shown that it can effectively and efficiently deliver vaccines to populations. However, never before has this volume of vaccines been required to vaccinate such a large number of people, at once. The delivery of the required doses of the COVID-19 vaccine will face challenges, requiring the implementation of innovative delivery mechanisms, especially to reach the last mile. This may be further complicated if vaccines need extreme storage conditions such as -80 degree freezers.

(8) Who should be prioritized for an eventual COVID-19 vaccine?
All countries are required to put in place an ethical distribution framework once a vaccine that is safe and effective becomes available. Countries have to decide to prioritise, i.e. those that are most vulnerable to severe illness, such as the elderly, people living with chronic illness given their risk of having a severe illness and potentially death. Another obvious priority group are frontline health workers because of their risk of contracting of the virus. Health workers need to be protected, giving their critical role as first responders safeguarding the country’s health security and caring for patients who have contracted COVID-19. WHO is supporting countries in identifying a prioritisation framework with the development of an allocation framework with an equity lens, focused on fair access to a COVID-19 vaccine through the COVAX facility. This is being supported by the Strategic Advisory Group of Experts on Immunisation (SAGE), applying the Values Framework.

(9) Is Nigeria building the capacity to develop vaccines?
Nigeria is still at the early stages in playing a critical role in vaccine development. When the first cases of COVID-19 were confirmed in China, Nigeria was the first country in Africa to carry out genomic sequencing of SARS-CoV-2, the virus that causes COVID-19. The African Centre of Excellence for Genomics of Infectious Diseases (ACEGID), inside Redeemer’s University, Ede, Osun State is building capacity in genomics, which is a precursor to vaccine development.
Funding for clinical trials within the country continues to present a challenge, despite the Central Bank of Nigeria’s framework to help researchers, biotechnology firms and science institutions access funds for research and development into therapeutics and vaccines to prevent the spread of COVID-19. However, the underlying issue of underinvestment in our science research capacity and the low prioritisation of Science, Technology, Engineering, and Mathematics (STEM) in our school curriculum and higher education institutions risks holding the country back in its push to grow it capacity for science.

(10) Why COVAX is a great example for multilateralism?
The world is waiting for a vaccine that will provide protection, and there is measured optimism about an imminent vaccine that low-income countries will have access to, but there remains a lot of concern. There needs to be a fair distribution of vaccines, if infectious diseases are really considered as a global health security threat and vaccines really considered as a global public good. This will require global leadership, multilateralism and transparency, explaining the science and potential side effects and benefits of an eventual vaccine.
So far, there has been a lot of solidarity, especially through the COVAX facility. This was a lesson from the H1N1 outbreak when African countries were not excluded in the supply pipeline of the H1N1 vaccine. There are strong calls for global unity, as until all countries are safe, no one country is safe. While there has been a lot of nationalism around access and availability of a COVID-19 vaccine, there is an emerging consensus that affordability should not define access to vaccines in 2020. The COVAX facility could also serve as a model for future equitable vaccine procurement.