I have been on a social media break, which just happened to coincide with the unfurling of the COVID-19 phenomenon. Peeking briefly into Twitter last week, I was stunned at some of the reactions I was seeing in relation the COVID-19 pandemic. It led me to want to share a few personal reflections as a public health physician working to plan for and manage outbreaks over two decades in different parts of the world. More importantly, these come from my reflections as a fellow human being, at a time of challenge for us all. I do not in any way intend by these thoughts to minimise the seriousness of the challenge the whole world faces, but I hope they may perhaps be of value to some people.
Over the last 18 months, I have been trying to use the Serenity Prayer to guide my actions and reactions to events in my personal life and the wider world. This followed a realisation on New Year’s Day in 2019, when, on a beach surrounded by laughing families, strolling lovers, and happy friends, I watched the sun dip into the Atlantic Ocean. At that moment, I realised that the social developments I had spent the previous year agonising about would one day pass. There would be turbulence and suffering, and many lives lost, perhaps including mine, but in a decade or two, many of those concerns would only be memories to the people who, on a New Year’s Day in 2034, would be strolling that same beach.
For those not familiar with the prayer, which I think is useful whether you have faith or not, it goes:
I have found it very helpful for maintaining my mental health as I deal with the turbulence in the three countries I have personal connections to; the United Kingdom (UK), Nigeria and the United States (US) over the past few years. It was also helpful when I lost my laptop earlier this year, having left it on a train. Thanks to Transport for London, I got it back.
I have also found it very helpful at this time of COVID-19, in looking at the things I can change and the things I cannot.
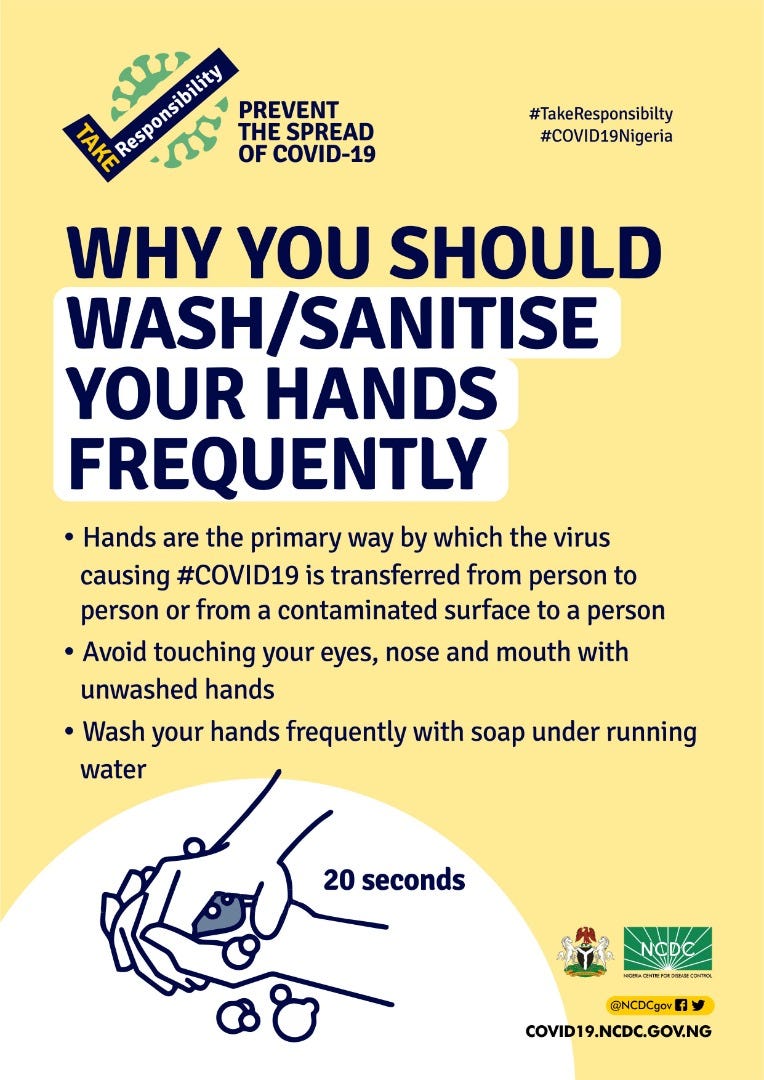
So, I can choose to follow the advice from public health authorities and try to modify my behaviour accordingly and encourage others to do the same. I can choose how much time I spend on social media, which messages I share and how I spend my time.
Following advice from public health authorities may limit my chances of getting infected, but it will not guarantee that I will not get infected. It will not determine the course and outcome of the illness if I do get infected.
As I contemplate the unprecedented disruption to our way of life and see the livelihoods of people threatened, it feels apocalyptic. But then I remember my parents who left Cambridge in 1966 to go and help build up the young university of Nigeria in Nsukka, and who by 1968 were fleeing war, as refugees, sleeping on bare earth, unsure of the next meal, taking cover from the bombs raining down from the sky.
I remember the sufferings of the people of Syria and the agonies faced by the people of Yemen, and these help me remember that self-isolation at home in London, although in a small space, with no toilet roll or pasta on the shop shelves, is not the end of the world. I am not a refugee, I am still at home. I can still eat regularly, perhaps not my favourite cereal or pasta but I can still eat good nutritious food, and though uncertain about tomorrow, I am not dodging bombs.
The courage to manage a disease outbreak
Outbreak management is a delicate, complex, fast-moving thing. Decisions are made rapidly against a constantly changing picture of events with incomplete information and many competing priorities to balance. Virtually every decision, no matter how carefully thought through, may result in some unintended consequences. No one ever completely gets it all 100% right, 100% of the time, but what you always want are people and institutions with the best knowledge, skills and experience firmly in charge, leading the response.
Having trained with and worked with so many public health colleagues currently working at Public Health England, I can confidently say there are few other people or organisations I would rather have managing an outbreak I was involved in, or living through.
Which brings me to Nigeria.

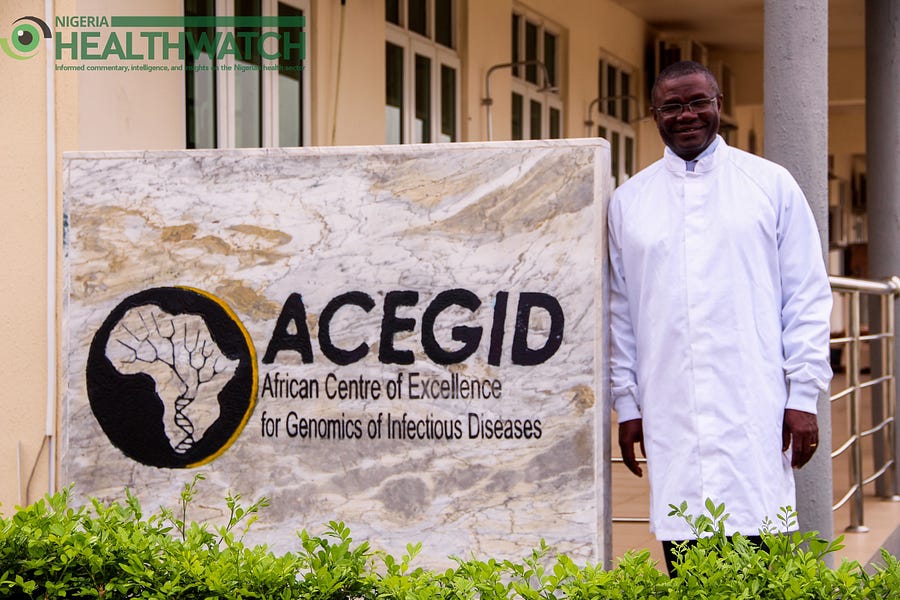
If there were just 10 epidemiologists in the world today, who could deliver the best possible in outbreak management, anywhere in the world, whether resource-rich or resource-poor, my brother Chikwe Ihekweazu would be one of them. He and his Nigeria Centre for Disease Control team, solidly supported by the Minister of Health, Dr Osagie Ehanire, are not infallible, but they are committed, dedicated professionals with a passion for public service and for Nigeria.
Looking more widely to Africa, we are in a much better place at this time, despite our fragile health systems, with seasoned African public health leaders in strategic places. People like Dr John Nkengasong at the newly established Africa CDC; Dr Moeti Tshidi at the World Health Organisation (WHO) AFRO office, Prof Stanley Okolo at the West Africa Health Organisation (WAHO) all supported by international partner organisations such as the UK Government project on strengthening the international health regulations led by my sister Ebere Okereke and her team, including Olusola Aruna in Abuja. With these people, the continent is in a better position to think through and respond to an infectious disease threat than ever before.
Let’s also factor in the training of cohorts of African field epidemiologists under the AFENET programme funded by the US, and the work of African scientists like Prof Iruka Okeke, former professor of molecular biology at Haverford College, now at the University of Ibadan, and Prof Christian Happi of ACEGID, who are training the next generation of scientists as covered by Nigeria Health Watch in November 2019.
There have also been positive developments in relation to building African capacity to tackle outbreaks such as the first ever full scale simulation of an infectious disease outbreak in West Africa in March 2018, which I was privileged to be lead consultant on.
This does not mean we should be complacent. The scale of the challenge is huge, and the cost in human suffering and lives is likely to be significant, but it’s worth remembering the little steps of progress that may make a difference.
Many people complain in different countries about symptomatic people being unable to access COVID tests. While this concern is understandable, testing changes little for the individual. If symptomatic, with a persistent dry cough and high fever, the advice is the same whether you test positive or negative, as there is no current curative treatment.
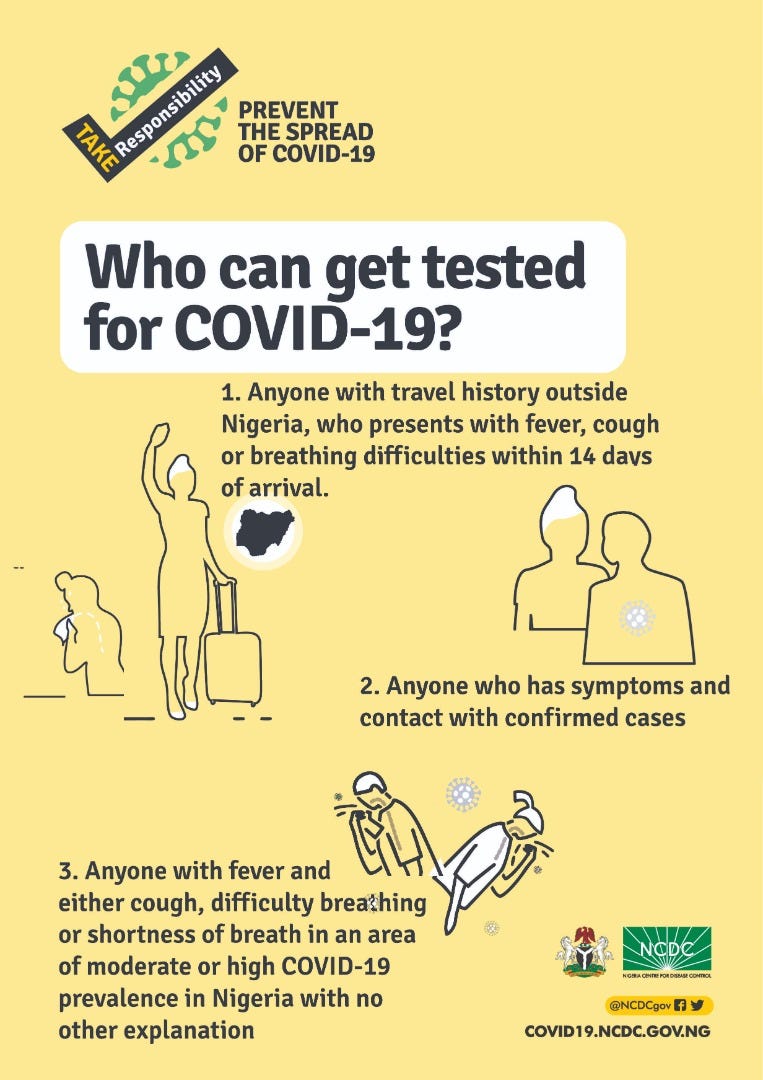
Testing is important from a population perspective to keep a handle on how an outbreak is developing, but very few if any outbreaks exist where we manage to test every single infected person. Usually there are always people with mild symptoms, estimated to be 80% with COVID-19, and many of these recover without seeking clinical help.
Many scientifically acceptable ways exist to measure disease burden and trends via sampling, so it is important to consider that while testing every case is ideal, public health needs to consider the best use of scarce resources. I know there are many people who want to help. May I suggest the best way to start is finding out what already exists so that you can plug in and liaise with others doing similar work.
The wisdom to make right choices for your health
With no intention of minimising the potential impact of COVID-19 and the importance of strictly following the public health advice to prevent its spread, it is also worth each of us asking, as I protect myself against COVID-19, how well am I following public health advice on other risks to my health, like cancer, cardiovascular disease, and road accidents? Because there are people worried about COVID-19 who will not be with us tomorrow, lost to other health issues they were not paying attention to.
Which brings me back to where I began: “…courage to change what we can, and wisdom to know the difference…”
So be safe, breathe, follow the guidance, only share information from trusted sources. Be kind, patient and supportive towards each other as we work together through this.
I’m going back to my social media break now… after I wash my hands for 20 seconds.




Thank you Ike for your wise words and for sharing your thoughts on the current situation that we are all facing around the world. The serenity prayer really rang true with me and my situation here in Wales UK, may everyone have it in the back of their minds as we face this epidemic…
Thank you once more and please stay safe everyone, and wash your hands!
Excellent piece Dr. Anya. You capture the highlights but my fear as a Nigerian as a dr is how far and how long shall the lockdowns and restrictions help us to contain the disease considering the heterogenous nature of our society
A call to serenity……
This article is lucid, imbibed with serenity and sincerity of purpose.
I have much appreciated reading the appeal behind the motivation to end at the point at which it started.
A professional with a heart describing the fragility of the human we are, we shall all die.
Thank you Doctor.
Thank you very much Sir…. But the problem right now is lock down, because people are dying of hunger
Fantastic piece here.
Enjoyed reading it and the very important link to my favourite prayer.
Thank you Dr Anya.
Indeed, Africa can… Guess we just need to believe in ourselves a little more and then see the big difference this will make.
This will surely pass… I know it will.
Thank you again!
Thanks for this informative piece. It’s always good to communicate hope and destigmatization. Awesome!