Since the declaration of COVID-19 as a pandemic by the World Health Organisation, Nigeria like most countries across the world has been battling to contain the disease. The Federal Government restricted flights from high risk countries into the nation’s airports and later followed with total closure. Total lockdowns were imposed by the Federal Government on Lagos and Ogun states, and the Federal Capital Territory (FCT). Many states have also imposed lockdowns, border closure or restriction of movement. New isolation centres are being built and existing ones are being upgraded. New laboratories have been established and others upgraded by the Nigeria Centre for Disease Control (NCDC) to carry out testing on samples of individuals suspected to be having the disease. Donations in kind and cash have poured in from individuals, companies and organisations to help the governments combat the pandemic. In addition, thousands of health workers are being trained by the NCDC on infection prevention and management as it relates to COVID-19.
While Nigeria is doing relatively well in terms of laboratories, isolation centres, contact tracing and strengthening of some tertiary health facilities, a critical opportunity is being missed especially by state governments to incorporate the strongest pillar of every health care system — the Primary Health Care System into the fight against COVID-19.
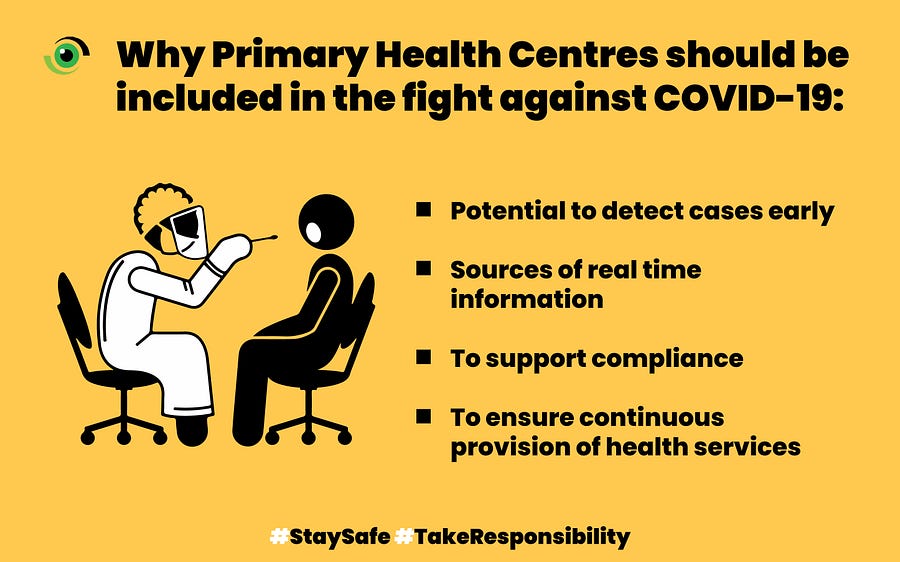
Primary Health Centres (PHCs) are mostly located in communities and should be health facilities in which community members seek for healthcare first. With majority of Nigeria’s population living in these areas and strong indications of community transmission of the disease, PHCs should serve as an important link in the management of the COVID-19. Here’s how:
Potential to detect cases early
Being closest care providers to the people in the community, health workers in PHCs are being trained by the Nigeria Centre for Disease Control and partners to maintain high index of suspicion while attending to patients. This should be intensified and taken to scale. As a result, they will be able to detect suspicious cases early enough as they present to the facility, and prevent community spread. Disease Surveillance and Notification Officers (DSNOs) at local government level could be alerted early enough, and the suspected individual could be isolated and tested. In the event the test results are positive, the health workers could assist in conducting contact tracing in the communities, as they are familiar with the people and environment.
Sources of real time information
Infectious disease outbreaks could be confusing for people. People often search for information and could end up getting false alarms. COVID-19 is no exception to this, as misinformation has been rife. Health care workers at PHCs could help dispel this by carrying out house-to-house visits to sensitise people about COVID-19 and emphasise on preventive measures. During the visits, they can carry out activities like teaching proper handwashing techniques and how to maintain social distancing. Being respected members of their communities, people are more likely listen to their advice and adhere to their instructions.

To supporting compliance
With majority of states under lockdown and security agencies helping in enforcing it, health workers can complement the work of the police and other agencies in rural areas. The number of security agencies are clearly not enough to enforce the rules in every nook and cranny of the country. Health workers can help ensure that people in rural communities do not engage in social gatherings such as naming and wedding ceremonies, as well as religious gatherings. They can do this by advocating to community and religious leaders through the Ward Development Committee, an influential community development group which usually has PHC workers as members. PHC workers should also reach out to youth and women groups in communities. They can pass the needed information and advocate for adherence to preventive mechanisms.
Ensure continuous provision of health services
Even as the country grapples to control the COVID-19 disease, health care facilities including PHCs should continue to provide care to the people. In the communities, PHCs should be encouraged to continue providing services like immunisation and antenatal, although these services should be provided in ways that ensure physical distancing. Through that, community members would have more confidence in the primary health care system, and they will be encouraged to present to health facilities to seek healthcare. The PHCs could also use the period of the services to provide counselling on COVID-19 and preventative methods to their clients, who will in turn pass the messaging to their relatives at home.

Nigeria’s stretched health system requires every hand on board
If there is anything COVID-19 has taught us, it is that our entire health system can be stretched to its limits with just one major emergency. It has amplified the need for continuous strengthening of healthcare facilities and institutions. As emphasised by the Partnership for Advocacy in Child and Family Health at Scale (PACaH@Scale, the fight against COVID19 should not be one which de-emphasizes PHCs against a specialized and central command system of service delivery. Admittedly, response to COVID19 requires highly specialised interventions mostly carried out at tertiary health facilities and specialised laboratories. However, the role of PHCs in overall prevention and response to outbreaks cannot be overlooked. Here, symptoms could be detected early in communities and relevant authorities could be alerted early enough.
According to reports from the Risk Communications team of the COVID 19 containment, the NCDC has trained State teams on risk communications across all 36 states. These teams are then charged with providing state level leadership to ensure that LGA teams, PHC teams and Community Mobilisers are trained. NCDC has also trained military and para-military personnel on risk communications, to strengthen reach of messaging in military communities, leverage the strength of the military to take messaging to security compromised areas and to ensure that front line paramilitary staff charged with enforcing the lockdown take on a sensitisation approach in delivering their mandate.

The National Primary Health Care Development Agency (NPHCDA) which provides oversight over the country’s primary health centres, should provide guidelines and coordination during this outbreak. Reports from the Risk Communications team of the COVID-19 containment note that the NPHCDA is currently training primary health care teams, using a comprehensive module that includes risk communication but also centres on infection, prevention and control at PHCs and ensuring that essential services remain available to communities.
To defeat COVID-19, we must halt community spread and to do that we have to ensure our PHCs are strong enough to provide both preventive and referral services in communities.
How else can PHCs be involved in the fight against COVID-19? Share your comments with us on our social media platforms, @nighealthwatch on Twitter and @nigeriahealthwatch on Facebook and Instagram. You may also leave a comment below.



One area of concern for the fight of COVID19 is the presence of water supply, sanitation and hygiene facilities in PHCs……what is your observation or finding on access to safe water, sanitation and hand washing in these PHCs.
Thank you.
Sir toilet r too dirty and not hygiene. Once a day staff come and clean. Toilet chamber totally full bad smell everywhere since yesterday evening. So pls help us. Tell to ur staff clean toilets time to time.
Apart from that everything perfect.
Is thre a role for retired healthcare providers in the Covid 19 prevention and,evaluation and management.
Thank you for this exposé on the place of PHCs in the COVID-19 fight. The neglect of the PHCs by governments at all levels, especially the States that have subdued the local government system, has made the prevention and control of COVID-19 look special and difficult. This has brought all manner of players to the field, with it’s confusing components.
The Community Disease Surveilance System is neglected but should be strengthened to help with effective detection, reporting, referral and contact tracing.
The PHC workers should be central to the control of COVID-19, and all communicable and non-communicable diseases. There should be for every local government a Medical Officer of Health whose duty it is to coordinate healthcare provision at the LGAs.
The COVID-19 pandemic provides Nigeria the opportunity to revitalize and strengthen the PHCs for better health outcomes for the citizens.
Yours is well written and i personally agree with your concerns, the NPHCDA is on top of this and all states are working with NPHCDA in training of PHC workers to respond to COVID-19 with support from Government and partners.