By Kemisola Agbaoye (Lead Writer)
Malaria is one of the leading causes of death in children under five years of age globally. According to the World Health Organisation (WHO), a child dies from malaria every two minutes. Eighty percent of the global malaria burden is carried by 15 countries, 14 of which are in Sub-Saharan Africa. Malaria is caused by the Plasmodium species and transmitted by infected female Anopheles mosquitoes. WHO describes malaria elimination as the interruption of local transmission of a specified malaria parasite species in a defined geographical area because of deliberate activities, and it is a global health priority that is central to the achievement of the Sustainable Development Goals (SDGs), particularly SDG3.
The road to Malaria elimination
According to the WHO, there are four phases of malaria elimination in a region or country; control, pre-elimination, elimination, and prevention of re-introduction.
To go from control to pre-elimination, less than 5% of suspected cases in that country should be confirmed to be malaria. To go from pre-elimination to elimination, less than one in 1,000 cases of malaria should be reported per year. To go from elimination to prevention of re-introduction, there must be no malaria cases transmitted by mosquitoes for at least three consecutive years, at which point the region or country is certified malaria-free by the WHO.
As of February 2021, a total of 98 countries had been certified malaria-free by the WHO and few African countries attained this milestone — Algeria (2019), Mauritius (1973), La Reunion (1979), Lesotho (2012) and Seychelles (2012). Two of these five countries — Lesotho and Seychelles — either did not do anything specific to achieve elimination, or never had malaria in their history.
The road to elimination differs significantly across regions and countries. Malaria was eradicated in Europe in the 1970s through a combination of insecticide spraying, early diagnosis and treatment and environmental engineering. The fact that mosquitoes in Europe have a shorter life span, are less attracted to human hosts, and that winter temperatures are inconducive for parasite development, made it easier to achieve eradication in Europe. In Central America, El-Salvador, which was certified malaria-free in February 2021, deployed a multi-sectoral, collaborative mechanism that included a strong vector control program, community involvement and rigorous testing. Trained community volunteers identified, tested, and referred suspected malaria cases for treatment, thus actively boosting their malaria surveillance measures. Achieving this feat is particularly impressive, given that El-Salvador is in a tropical region and quite like countries in Africa where elimination has proven very difficult. The most recently certified country in Africa — Algeria in 2019, employed free malaria testing and treatment, well-trained healthcare personnel, quick outbreak response and improved surveillance measures.

Once elimination has been achieved, countries must prevent re-introduction of transmission. La Reunion, an island in the Pacific Ocean just off Madagascar, achieved elimination through aggressive campaigns that included Indoor Residual Spraying (IRS), spraying of breeding sites, active case detection and mandatory reporting by health care facilities. It has prevented re-introduction of transmission for over 40 years, employing measures like passive case detection and early treatment of imported cases and a larval control programme guided by rigorous vector surveillance.
Nigeria’s current reality
Nigeria carries 25% of the global Malaria burden. Since 2013, the National Malaria Elimination Programme (NMEP) has been responsible for the oversight and management of all malaria control programmes and activities in the country. The National Malaria Strategic Plan 2014–2020 outlines the country’s malaria elimination objectives and five key interventions, which include universal access to Long-Lasting Insecticide-treated Nets (LLINs), IRS, Larval Source Management (LSM), provision of Intermittent Preventive Treatment of Malaria in pregnancy (IPTp), vector surveillance and resistance monitoring and quality assurance of commodities.
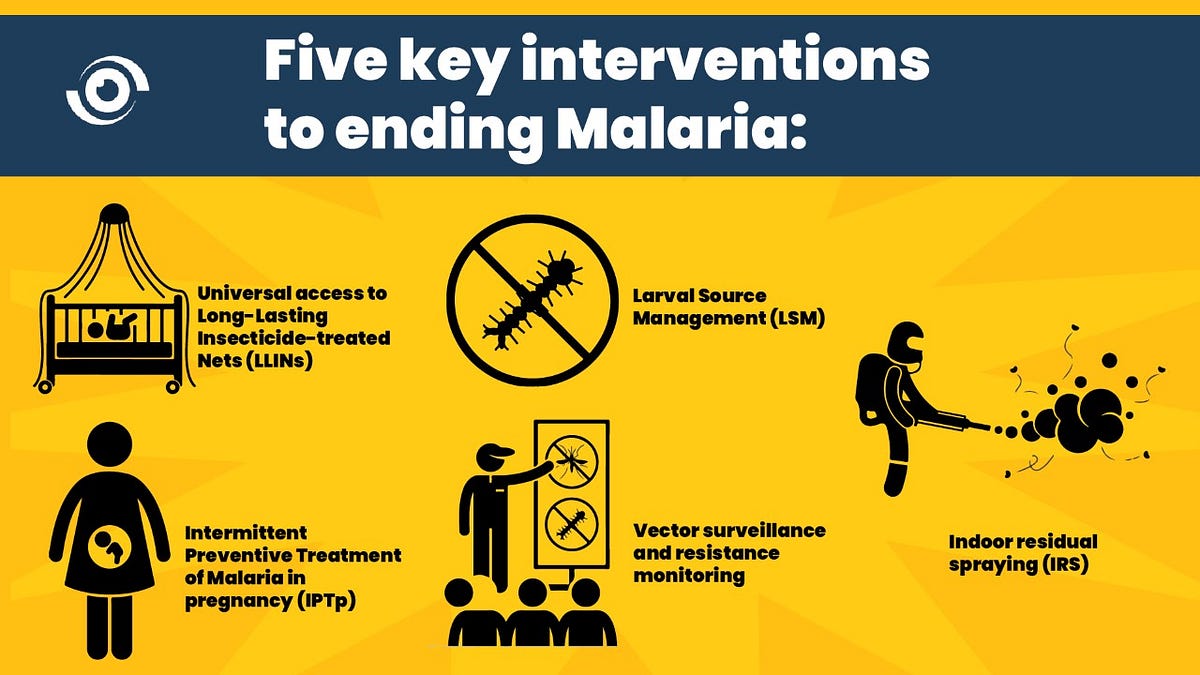
While LLINs are effective in prevention of transmission of malaria in sub-Saharan Africa and there have been substantial efforts to promote its use among Nigerians, utilisation of the nets is still quite low. This could be because most Nigerians are still resistant to sleeping under a mosquito net.
IRS is a process where the walls, ceilings and other surfaces of a house are coated with long lasting insecticides to kill any mosquitoes that perch on the surface. It is considered very effective in interrupting transmission, but it is not commonly done in Nigeria. According to the 2015 Malaria Indicator Survey (MIS) conducted in 2015, only 1% of the population had IRS done in the last 12 months. This may be due to the high cost of conducting IRS campaigns, the increasing resistance of mosquitoes to insecticides, and inadequate vector mapping to guide implementation.
Larval Source Management is useful for the control of breeding sites only when they are few, fixed and findable, which might not be the case in most Nigerian communities. There has also been a low uptake of IPTp with only 19% of the population receiving 3 doses as of 2015, though this proportion may have increased since the last MIS.
There has been a significant improvement in malaria diagnosis and treatment at health facilities. Between 70–90% of fever cases reporting to health facilities are being tested for malaria, and the availability of Artemisinin Combination Therapy (ACT) in the country is up to 97%. There is, however, still a high incidence of over the counter treatment of the disease which undermines efforts to improve testing and diagnosis. This begs the question, should over the counter treatment of malaria be banned, as recommended by WHO? Is there sufficient public confidence in our available diagnostic and treatment services to ensure that people will access care at health facilities instead of buying over the counter antimalarial drugs for self-medication?
What can we do better in Nigeria?
In addition to stronger malaria surveillance, diagnostic and treatment services, Nigeria needs to improve its vector control programme if it is to progress more quickly towards malaria elimination. Vector control has been proven to successfully reduce or interrupt malaria transmission when coverage is high, and as seen in most countries or regions that have eliminated malaria, it is key to the prevention of re-introduction. To strengthen our vector control programme, we need to design and implement targeted behaviour change communication interventions to increase utilization of LLINs and invest more in IRS, vector surveillance and insecticide resistance monitoring. There is also an urgent need to address the overarching deficiencies in data collection and reporting; we need current data to inform the design, review, and implementation of malaria control policies by policy makers.

Can improved WASH services strengthen malaria control?
Community-based interventions targeted at increasing knowledge and awareness of the importance of proper Water, Sanitation and Hygiene (WASH) services in reducing malaria transmission have been proven to be beneficial, particularly as part of larger WASH campaigns for prevention of childhood illnesses like diarrhoea. Simple recommendations, such as getting rid of mosquito breeding sites like old, discarded tyres, ensuring water storage containers are covered, maintaining a clean environment, and ensuring availability of potable water to reduce the need for water storage can add to mosquito control.
How can we advance more quickly towards Malaria elimination?
On this World Malaria Day 2021, let these recommendations serve as a call to action to all parties involved — the government, private sector, communities, and individuals. We have a long way to go to reach the zero malaria target.



Excellent – well written article.
This is a well researched health article; it is very educative health in terms of health education. Keep it up.
Good read.
Ecology and infrastructure around human settlements in Nigeria are significant barriers to elimination.
Vaccination seems to required silver bullet.
Marvelous!
I think commitment and attitudinal change is also very crucial.