By Ibukun Oguntola and Dara Ajala-Damisa (Lead Writers)
According to the 2018 Nigeria Demographic Health Survey (NDHS), there are 512 maternal deaths for every 100,000 live births.
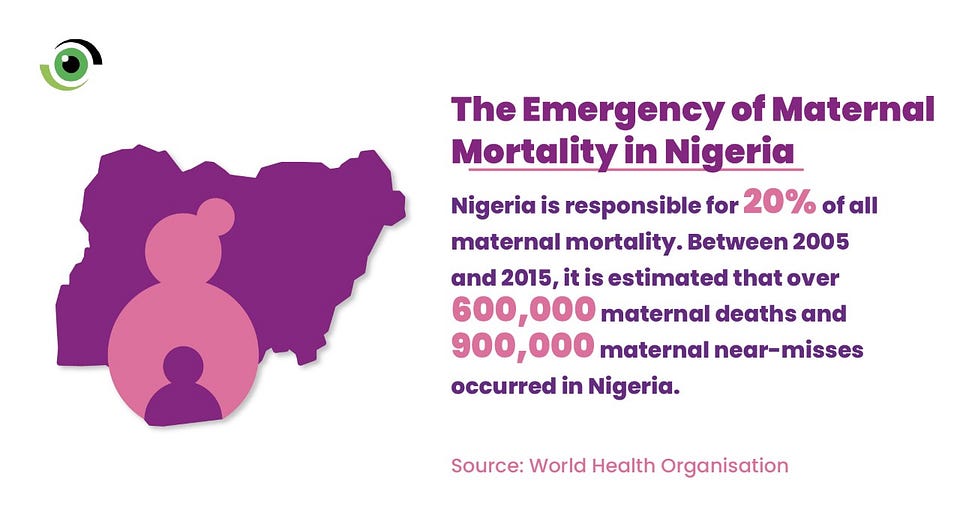
Nigeria accounts of 20% of global maternal deaths and between 2005 and 2015, it is estimated that 600,000 maternal fatalities occured and there were no less than 900,000 maternal near-misses. Heavy bleeding also known as postpartum haemorrhage (PPH), accounts for 23 percent of all maternal fatalities in Nigeria, followed by infections following childbirth (sepsis) at 17 percent and unsafe abortions at 11 percent. Many of the deaths are preventable and when women have access to effective care and medicines during labour and after childbirth, their outcomes are greatly improved, especially in the prevention of postpartum haemorrhage, the leading cause of maternal deaths in Nigeria. Access to quality care and essential medications is not only a human right, but it is also critical to achieving the United Nations’ Sustainable Development Goals (SDGs).
Paucity of data for action
In Nigeria, gaps in policies for medicine procurement contribute to the adverse outcomes of women when giving birth because they do not have access to quality, lifesaving medication. Women in especially hard-to-reach communities are hardest hit when accessing quality healthcare and medicines. Policy gaps exist in Nigeria’s national drug procurement landscape and the issues include the proliferation of substandard medicines as well as poor service delivery. Identifying and addressing these key policy gaps are important first steps in ensuring that medicines that are used for a woman while giving birth are of the right quality and potency to save her life and that of her unborn child, as well as enabling her to have a full recovery after giving birth.
Bridging the quality gaps
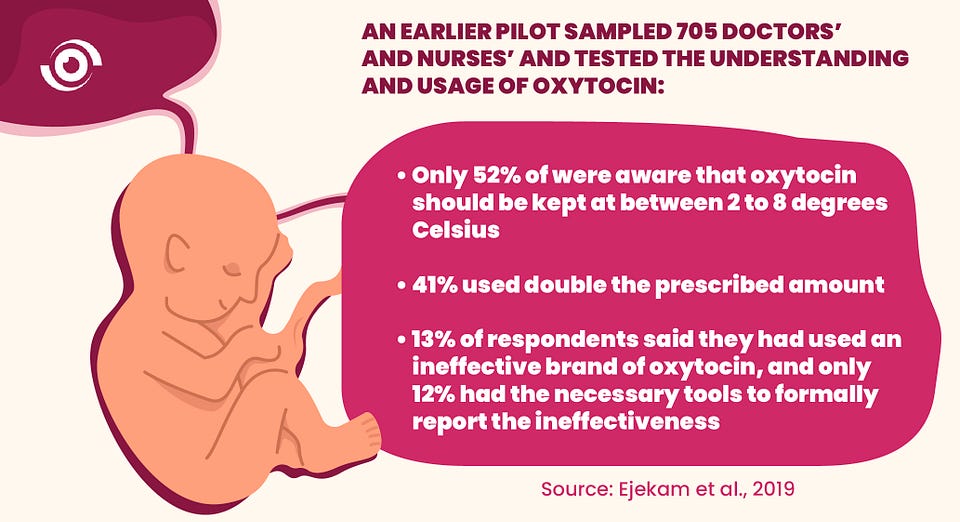
A 2018 study investigated the quality of medicines for maternal health in Nigeria. It reported that 74% of oxytocin samples failed laboratory tests. This meant there was a high prevalence of substandard oxytocin being used in the country. A pilot study in Lagos uncovered knowledge gaps in healthworkers when it tested 705 doctors’ and nurses’ understanding and usage of oxytocin. Only 52% of those polled were aware that oxytocin should be kept at temperatures ranging from 2 to 8 degrees Celsius — and 41% used double the prescribed amount. About 13% of respondents said they had used an ineffective brand of oxytocin, and only 12% possessed the necessary pharmacovigilance form in their health facilities to report the ineffectiveness.
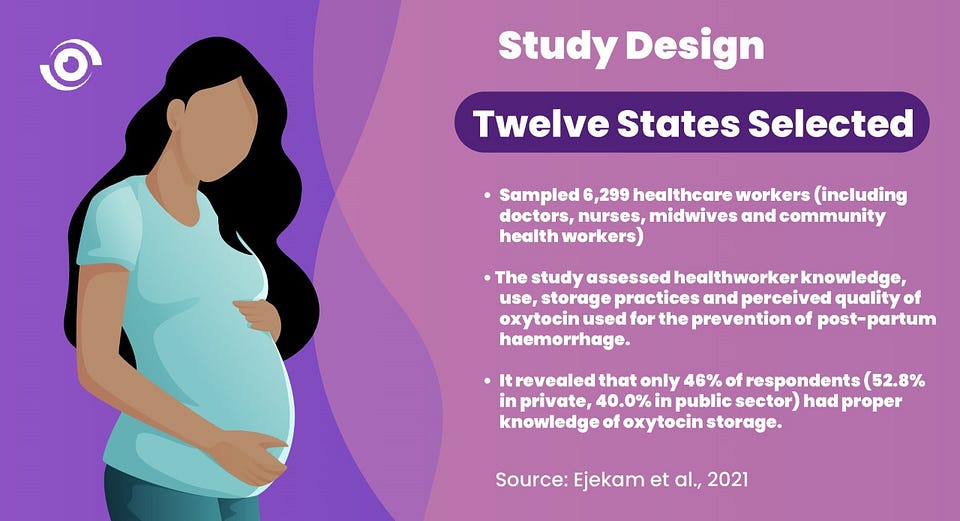
There was an urgent need to broaden the research to a larger representative sample of healthcare providers across the country, that directly administer oxytocin, in order to assess and understand their knowledge, usage, storage practices, and perceived quality and effectiveness of oxytocin in the prevention of post partum haemorraghe in Nigeria. To address this, a larger study was carried out assessing knowledge around oxytocin, usage, storage practices and perceived quality of oxytocin used by healthcare providers across Nigeria. Twelve states were selected and a sample of 6,299 healthcare workers (including doctors, nurses, midwives and community health workers) were assessed. The study revealed that only 46% of respondents (52.8% in private, 40.0% in public sector) had proper knowledge of oxytocin storage.
These studies provide evidence for the need to strengthen procurement processes and storage of maternal medicines in Nigeria. Further findings from the descriptive cross-sectional study also provides evidence for the need to increase the capacity of health workers in the storage and usage of oxytocin through continuous professional development in line with protocols for the management of PPH. The findings from the studies should be used to establish clinical guidelines, as well as serve as a guide for infrastructural development.
Evidence to policy
Using research findings to inform policy is critical, especially where it can contribute to improving health outcomes. Similar to most research studies, there were limitations to the descriptive cross-sectional study that could be addressed with further research. An example was the descriptive study across 12 states which was self-reported, so there was a possibility of recall bias on prior experiences. A qualitative study to supplement the quantitative data could be carried out in order to delve deeper into the concerns about the usage of oxytocin during labor and delivery.
Policy makers need evidence to inform their decision making. Advocacy must be evidence-based and seek the most effective ways to build on the available research evidence to influence policy and inform the media and the public.
Policy action can always be strengthened by accurate and relevant evidence. Evidence-based policy-making ensures that resources are used more efficiently and better targeted. It is important that while the Nigerian government is implementing programmes to enhance the health of its citizens and putting in place health interventions, policies and programmess need to be influenced by appropriate evidence in order to ensure that commensurate resources are allocated to the different areas of health to improve health indices.
What’s next??
Employing an evidence for change approach to bridge quality gaps in regards to access to maternal medicines will mean that policymakers leverage available evidence to improve policies and strengthen human resources for improved service delivery and procurement for maternal medicines across states.
Research also helps to provide direction for action plans, based on evidence. It has now become the responsibility of state governments and other relevant stakeholders to develop strategies that will include the development of clinical guidelines and regulations on the use of oxytocin, and continuous training of healthcare providers, especially nurses and midwives, on the proper use and storage of life-saving medicines to prevent adverse maternal outcomes.
Bridging the evidence-practice/policy gap is crucial in ensuring that significant knowledge gaps are plugged and learnings used to develop best practices that ensure alignment with health systems and human resources strengthening approaches. This would go some way in improving maternal health outcomes and indices in Nigeria.



In a country where there is no power supply, no diesel or fuel to power alternative source, how do you expect storage of oxytocin to be strictly adhered to even if you want to try? Even from manufactures end, have they maintained the cold chain before you purchase the drug.. we are in dire straits.