In May 2020, criticisms against a 22-year-old mother, Olufunmilola Adisa, accused of killing her baby in Lagos State flooded the internet. Reports alleged that she wrote a letter describing how she did it.
However, two individuals looked beyond the headlines and outpouring of condemnation and offered to assist Adisa. For Ahmed Adetola-Kazeem, a lawyer and founder of Prisoners’ Rights Advocacy Initiative (PRAI), offering this help was at the heart of their work, providing pro bono legal and rehabilitation services for inmates. For Onyedikachi Ekwerike, a Clinical Psychologist and founder of Postpartum Support Network Africa (PSN Africa), he knew it was a severe case of Postpartum Depression (PPD), something he has dealt with before, inspiring him to found PSN Africa.
“I got interested in maternal mental health in 2014 after a relative suffered postpartum psychosis. The whole confusion that it caused within the family and how poorly it was handled got me really frustrated with the lack of access to care for her,” Ekwerike said.
So he worked with Adetola-Kazeem to not only get legal representation for Adisa, but also mental health support as a patient, something his team at PSN Africa has been doing for other women since their inception in 2015.
An elusive problem
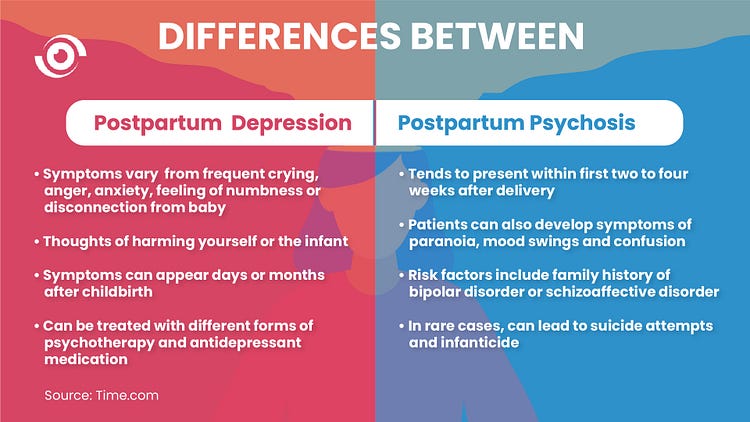
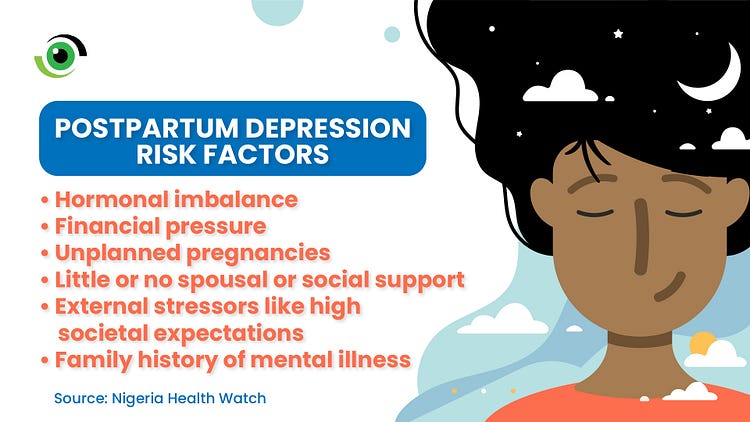
From mood swings, anxiety, irritability, unexplained sadness to hallucinations in severe cases, women experience PPD just like any other illness irrespective of their socioeconomic status. From university educated to development professionals, the experiences of dealing with perinatal or postpartum depression can be experienced by anyone. Dr Saratu (not real name), a medical doctor, shared her experience while reacting to Adisa’s case.
“Postpartum mental illnesses are real and even worse is the relatively poor understanding our society has. I have seen repulsive comments from seemingly educated people online on this issue,” she said.
“After my first child, the sleep deprivation alone tipped me. I would burst out in tears because I was so sleepy and there was this tiny thing that wouldn’t allow me. I even had social support. Even when there was someone to tend to her, I felt it was unfair to her to sleep while she was awake.”
“I pray Funmi gets the help she needs. It could be anyone,” Dr Saratu said.
It’s even more confusing that PPD can hide in plain sight as a woman can experience subtle symptoms, which prevent people from noticing the problem immediately.. The World Health Organisation (WHO) estimates that 19.8% of women experience postpartum depression in developing countries, with manifestations differing in severity.
Starting Somewhere
“Why did nobody tell me that I could become depressed after childbirth when I was pregnant or even before I got pregnant? How come nobody told me in the hospital when I was going for antenatal and postnatal? Nobody mentioned all these things to me.”
These were the questions asked by the second PPD patient Ekwerike came in contact with after his relative. She was the wife of a friend and he had to schedule home sessions to attend to her. Luckily, hers wasn’t as severe as his relative’s.

WHO recommends asking mothers about their emotional well being at each postnatal contact with health workers. They should also be asked about access to social support and coping strategies for everyday issues. However, this isn’t always the case as this first time mother said “Nobody asked how I felt”. In 2019, Meghan Markle, Duchess of Sussex revealed that she had struggled with postpartum depression after her first pregnancy and mentioned in an interview that no one had asked her if she was “ok”.
So PSN Africa started here, raising awareness about postpartum depression in health facilities across Lagos State. Ekwerike drafted an intervention plan which included education, screening and support for pregnant women. “But I knew that there was no way to make progress on a challenge as huge as this alone. I looked for who might be the stakeholders here, to help raise awareness at hospitals, to find these moms, who are our target audiences, and help them understand what these conditions are”, he said.
Due to the lack of access to antenatal clinics, he searched within his network to not only find like-minded people who could help refine the idea, but also provide a launchpad for their plans to take off. This was especially important because they were fresh out of training as clinical psychologists and had no track record. So it was important to gain the trust of the medical directors of the hospitals they identified as stakeholders.
Then the breakthrough came. His friend, Babatunde Oni connected him with his father, Dr Kunle Oni, in charge of a general hospital at the time.
They would later go on to clearly articulate interventions into five steps after feedback from women and experience from implementing over time. They focused on:
- Emotional intelligence training for nurses
- Educating pregnant and new mothers about PPD during antenatal and postnatal clinic days
- Screening test using the Edinburgh Postnatal Depression Scale (EPDS)
- Therapy both in groups and home visits
- Road 2 Recovery (R2R) support groups where women help each other through shared experiences.
A snowball effect
PSN Africa’s earlier efforts succeeded because of people who believed in their vision. After meeting with Dr Oni, he agreed that raising awareness about PPD and screening women was long overdue. He provided access and support for them to start. This gave the young organisation credibility to approach other hospitals with evidence of what they had done. “He was willing to put his name on the line for us by giving us notes to other hospitals. I like to point to him as the catalyst to the work we do,” Ekwerike said. He said from the first hospital, it became a snowball effect as they’ve visited almost every general hospital in Lagos State.
Letting other people with shared vision take the lead is another reason they succeeded. “PSN is an organisation driven by the people and my role is just facilitating an environment where people can work together and make progress on our goals,” Ekwerike said. He goes on to talk about Dr Ijeoma Idaresit, founder of Edie and Amy, a Nigerian and UK trained Medical Doctor who learned about PSN Africa’s work from Instagram, volunteered with them a few months after delivery and later took on bigger responsibilities in the organisation. “So for Dr Ij, I think it was the vision that drove her,” he said, adding that a mother who bought into their vision also donated all the three offices they’ve used in the Ikeja part of Lagos.

Dr Idaresit said she was drawn to PSN Africa’s work after seeing their outreach to hospitals talking about postpartum depression “because their approach was story-based, very compelling and because I understood. I don’t really think I was depressed but I really connected. I reached out and I joined them for an outreach at Lagos Island Maternity hospital and it was very fulfilling for me. From there, we went for some more outreaches and later, I joined the board”. She has been part of their major successes since joining them in 2017, including planning for their first World Maternal Mental Health Day Conference in 2018 where women shared their experiences of dealing and receiving help with PPD through PSN Africa.
Leading for change, growth and sustainability
Dr Idaresit managed the treatment intervention plan of the organisation, moving it online in 2020 because of the COVID-19 pandemic. The online support group, called Warrior Mom’s Village is facilitated by two clinical psychologists who provide virtual therapy sessions, content for the mothers and also have general sessions where mothers share experiences and get feedback from their peers. Before adding them to the groups, they are first sent an online form. The data is used to screen and categorise them after assessment. On what inspired the name, Dr Idaresit said “All the moms that we’ve helped are warriors. They fought for their children and for themselves. So we termed them as warrior moms. When we thought of having a virtual support group and realised it takes a village, we decided it’s going to be a warrior mom’s village because we have fighters and survivors there that thrived despite everything. That’s why we call them warrior moms. They are not victims, they are champions.”
One of their most profound stories of impact is Mr Henry (not real name), a Lagos based lawyer who reached out to them in 2018. Researching some of his wife’s symptoms and suspecting PPD, he looked for organisations that provided interventions in Nigeria. After six weeks of therapy and antidepressants prescribed by a psychiatrist, she improved. “The husband was surprised after the first home session I had with her as she started engaging better than before. He said he didn’t believe such services were available in Nigeria”. Now he offers pro-bono legal services to the organisation as a way of supporting their work and showing his appreciation.

Dr Idaresit’s biggest lesson working with the organisation is that “relationships are everything.”
“A lot of PSN Africa has been built on relationships with colleagues, other partners, nurses and medical directors, not necessarily funding,” she said. To scale however, she agrees that funding is required. They received their first grant from the ACT Foundation to do more work and so far, they’ve educated up to 16,000 people and screened about8,000 mothers in 50 government hospitals across Lagos and Ogun States, providing treatment for about 500.
Screening is the easy part, Idaresit said. Treatment is more challenging as it’s expensive. Half of the amount used to screen a thousand women can be used to provide treatment for just one woman. The initial challenge was lack of screening after education but when screening and case identification began, treatment became another challenge as the clinical psychologists they worked with couldn’t attend to everyone.
Another challenge is the fact they are providing the screening themselves. “This is an aberration. We shouldn’t have outsiders coming into the hospitals to carry out this kind of screening exercises. It should be part of the system. So what we are looking at now is trying to see how we can partner with the hospitals to institutionalise it into their regular operation,” Dr Idaresit said.
This will require policy intervention, says Ekwerike, and they are hoping Lagos State and other states pass a bill that mandates hospitals to screen women for signs of postpartum depression. This way, their work will focus on holding hospitals accountable and providing training where there are capacity gaps. He said this is a more sustainable way of solving the human resource challenge they face.

For Oluwafunmilola, Dr Idaresit is happy she’s getting the treatment she needs but feels sad because the fallout is permanent even after she recovers because the memory of her actions will remain. Advocacy must continue to ensure that other women who may suffer from PPD are identified and treated before they can harm themselves or their baby.
However, steady progress is being made. “We’ve moved from where we were in 2017 because there is now more talk about mental health and people are now more comfortable and more sympathetic. We still need to do more about our awareness but we are making progress,” Dr Idaresit concluded.
At the time of completing this story, it came to our notice that Dr. Ijeoma Idaresit passed away with her two daughters on 12 December 2020 in a domestic fire accident. The interview with her was done in June 2020. We at Nigeria Health Watch commiserate with her family, friends and team at PSN Africa.



This is truly beautiful. It goes to show how much of depression mothers face silently. This message probably needs to be taken to the low-income areas of Lagos as well as the primary health-centres where a number of our women attend for their ante-natal needs.
Kudos to the team