Hospitals have been at the heart of the spread of the Ebola virus from the first outbreak ever reported; but they are also at the heart of successful responses. A few days ago the Director of the CDC in the US said that the chances of the Ebola Virus spreading the US were virtually “zero”, not because of the existence of a vaccine or treatment but because of their good track record with Ebola in the past. The organization Medecins Sans Frontieres (Doctors Without Borders) has been on the frontline of the clinical response to almost all Ebola outbreaks; yet they have not lost a single colleague to Ebola. In this post, we examine why.
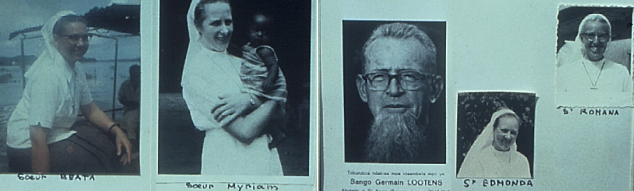
The first recognized outbreak of Ebola fever began in northern Zaire in 1976, on the banks of the Ebola River. The first patient was a 44 year-old male teacher, who went to the Yambuku Mission Hospital for treatment for an illness with fever which he believed to be malaria. He was given a chloroquine (anti-malarial) injection at the hospital, which at the time did not use disposable needles or sterilization of needles between uses. This led to a rapid spread of Ebola fever in the surrounding villages and among the hospital staff who cared for the initial cases. [1] The hospital was the source of infection for 4 weeks after the index case and was subsequently closed, 11 of the 17 staff members having died of the disease.
The subsequent history of Ebola disease outbreaks indicates that, in most cases, Ebola virus is introduced into human populations through some contact with infected animals. Later transmission is from person to person, with people most at risk being family members and health-care staff. [2] Hospitals often serve to amplify the infection in the community if the right effective infection control measures are not put in place rapidly.
There is evidence that rapid implementation of effective infection control measures in hospitals can have a significant impact in controlling the disease, as shown in an outbreak in Uganda, where the number of newly infected cases dropped dramatically after the institution of hospital isolation wards. [3]
Hospitals and health centres therefore form a crucial link in the control of an Ebola outbreak, and, given the knowledge that exists on effective infection control within hospitals, it is no surprise that Dr Thomas Frieden, head of the US Centers for Disease Control, is confident that a large outbreak will not occur in the US. In a recent statement to US lawmakers, he said “We know how to stop Ebola with strict infection control practices, which are already in widespread use in American hospitals.” [4]
If we know all this, why then has the disease continued to spread rapidly in the recent outbreak in some West African countries, and why have there been so many healthcare workers infected by the primary case in Nigeria? It is clear that the humid conditions, the challenging socio-economic environment and the general lack of education on infection control in the affected countries all contribute to making the practice of infection control difficult during “peace” time. As infection control measures have to become part of the “practice culture” to be effective, it is no surprise that, when an outbreak occurs in settings where these practices are not embedded, there will be some breaches, sadly in same cases with fatal outcomes.
The CDC recently issued updated guidance to US hospitals where travellers from regions with confirmed cases may present. Most of the steps are not particularly complex or expensive. They include messages such as:
Patients with known or suspected Ebola virus infection should be assigned a single-bed room, and consider posting someone at the patient’s door to ensure that all individuals entering the room consistently use the correct personal protective equipment (PPE). They should at least wear gloves, a fluid-resistant or impermeable gown, goggles or face shield, and facemask. Copious amounts of blood and other body fluids, vomit, or feces may require extra PPE such as double gloving and leg coverings.
Clinicians should limit phlebotomy, laboratory tests, and other procedures to the minimum necessary to properly evaluate and treat the patient. If possible, they should avoid aerosol-generating procedures such as sputum induction, intubation and extubation, and open suctioning of airways. If such procedures must be performed, clinicians ideally should conduct them in an airborne infection isolation room and take measures to reduce their exposure to patient aerosols.
Healthcare personnel who develop symptoms of Ebola virus infection, such as fever, intense weakness, vomiting, and signs of hemorrhage, after an unprotected exposure should immediately stop working — or not report to work — and notify their supervisor. Personnel who are asymptomatic after an unprotected exposure may continue working provided they receive fever checks twice a day for 21 days after the last known exposure.
The CDC also have a manual for infection control in African hospitals that takes into account the local context, developed from their experience on supporting the control of previous outbreaks. http://www.cdc.gov/vhf/abroad/vhf-manual.html
A similar statement was made in the UK by Professor Peter Piot who said that, even if someone came to the UK during the incubation period, infection control measures in Britain would prevent the spread of the virus.Professor Piot is the director of the London School of Hygiene and Tropical Medicine and was part of the team that first identified the virus. https://uk.news.yahoo.com/border-staff-unprepared-ebola-045202515.html#Gxmiupe
We have the tools; the question is: Are our governments, health workers and hospitals willing, ready and able to implement those tools? We must rally around them to achieve the level of competence needed within the shortest possible time.
Most of the patients currently being managed for EBV are in the Infectious Disease Hospital in Yaba, Lagos. Tolu Ogunlesi visited the hospital recently. What he saw says a lot about the health system in Africa’s largest economy; he described it thus:
“… I met a hospital almost in ruins. Dilapidated, forgotten, depressing … a Siberia of sorts for doctors.”
So, again, we appeal to our colleagues and the government to sit down and resolve their differences. Now is not a time for the various parties to dig their heels into entrenched positions. If there is one lesson we must learn from Mandela, Africa’s greatest hero, it must be that there is no situation too hard to negotiate. The one indisputable truth in the current scenario is that there will not be one winner and that the greatest losers will be the Nigerian people. It is time to lock up NMA, JOHESU and the FGN in a room and not let them out until they make the compromises necessary to reach a resolution and for all to demonstrate their commitment and rebuild the trust needed to tackle this outbreak effectively.
[1] http://web.stanford.edu/group/virus/filo/eboz.html
[2] http://www.ncbi.nlm.nih.gov/pubmed/23327370
[3] http://wwwnc.cdc.gov/eid/article/9/11/03-0339_article
[4] http://www.medscape.com/viewarticle/829615