Sabrina Charles and Billy Mawindo (Guest writers)
Editor’s note: For long, Traditional Birth Attendants (TBAs) have played and continue to play a key role in maternal healthcare. In the past, TBAs worked in the shadows, illicitly performing at-home deliveries and increasing the rates of maternal mortality in Sierra Leone. In this article, Partners in Health-Sierra Leone share how the organisation is empowering and enabling TBAs to work in partnership with the formal healthcare system in an effort to reduce the maternal mortality rate in Sierra Leone.
For many years, Sierra Leone ranked as one of the countries with the highest maternal mortality rates in the world. Recent data indicates that Sierra Leone experienced the steepest drop in maternal mortality on the African continent between 2000–2020, with the last three years showing the most profound improvement. The maternal mortality rate is driven by high-risk pregnancies, and obstetric complications like postpartum hemorrhage, hypertension, obstructed labour, and sepsis. While there is only an estimate of maternal deaths happening outside of health care facilities, evidence shows that at-home deliveries are strongly associated with a higher risk of maternal and neonatal deaths. According to the World Health Organization, the major complications that account for nearly 75% of all maternal deaths are predominantly severe bleeding after childbirth, infections after childbirth, high blood pressure during pregnancy, preeclampsia, eclampsia, complications from delivery, and unsafe abortions. However, health care providers can only identify, address, and record these complications if and when pregnant women present themselves at healthcare facilities.

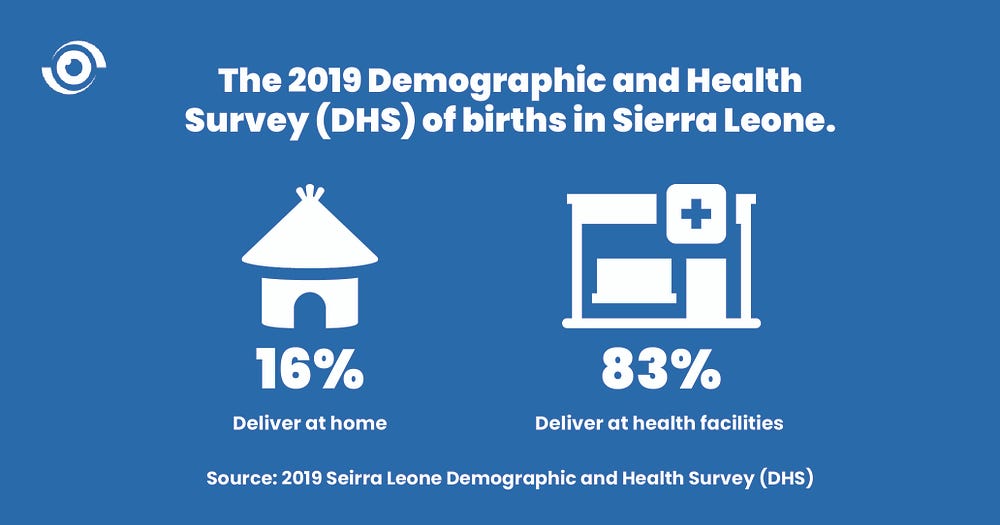
In 2019, the Sierra Leone Demographic and Health Survey (DHS) indicated that 83% of women in Sierra Leone delivered at health facilities and 16% delivered at home, though the difficulty with tracking the illegal practice of at-home deliveries is acknowledged. Kono District, where Partners In Health-Sierra Leone (PIH-SL) has a large presence and closely collaborates with the District Health Management Team (DMHT), once had one of the highest maternal mortality rates in the country at 8.9% according to the WHO’s 2016 Government of Sierra Leone Health Sector Performance Report. The combination of Kono’s rugged landscape, lack of basic resources, and a sometimes rational suspicion of health facilities contributed to poor maternal and neonatal health outcomes. In light of the numbers of preventable deaths occurring in the District, PIH-SL made comprehensive quality improvement investments in its Kono-based private clinic, The Wellbody Clinic, which thus far, has only experienced 1 maternal death between 2018 and 2023. Among other strategies, a key approach to improving maternal and neonatal health outcomes was in the ability to strengthen relationships between community members and local health care facilities. Enriched community engagement and enhanced health education improved care seeking behaviors, such as antenatal visits and facility-based deliveries. As a result of the positive experience, PIH, with the support and guidance of the Sierra Leone Ministry of Health (SL MOH) began scaling its approach to the only Secondary Care hospital in Kono District, the PIH-supported Koidu Government Hospital, which currently performs an average of 2,000 deliveries per year.
Building Trust
For long established reasons, many women across Sierra Leone have had a strong sense of trust and comfort with Traditional Birth Attendants (TBAs), particularly as it relates to maternal health and childbirthing. TBAs are highly regarded women in their communities, assisting mothers during childbirth though initially acquiring their skills through anecdotal guidance and experience sharing by older women in the community. Since TBAs are not clinically trained, and because they practice far from clinical settings which contain life-saving commodities, the risk of fatal outcomes during the labour and delivery process tends to be greater.
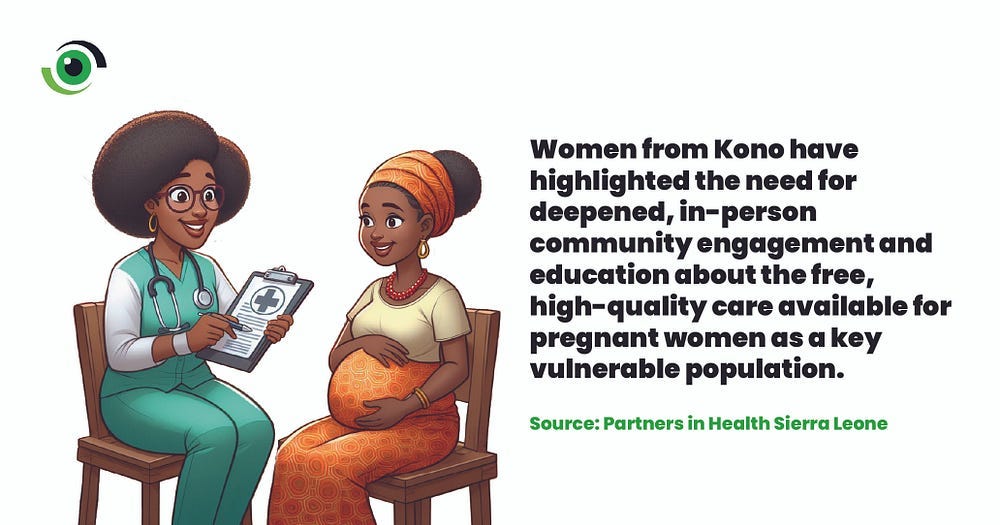
To increase levels of trust throughout communities in Kono, and to reduce the number of unsafe home births, investments were made in community engagement and system-wide mechanisms, especially those designed to acknowledge the meaningful role that TBAs play in their communities and on public health outcomes. Mabel, a woman from Kono, shared a sentiment echoed by other women in the District, that “some women still feel insecure and shy, there’s a lot of fear with women in the community” when it comes to facility-based care, which contributes to low rates of facility deliveries.

Kono women expressed discomfort with visiting hospitals without personal accompaniment due to historic perceptions of health care failures at the facilties. Women also mentioned the need for deeper, and more personal, engagement and education about the free high-quality care available to pregnant women. Many women were skeptical, or wholly unaware, that they are considered a key vulnerable population, and that the Government of Sierra Leone administers the Free Health Care Initiative (FHCI) which enables pregnant women, lactating mothers and children under five to access free-of-charge medical care and services. PIH-SL sought to bridge the gap between communities and health facilities by establishing the Wellbody Coalition, through funding from MSD for Mothers. Among other things, the consortium of international and local partners leverages community assets such as TBAs, introduces novel technologies, and reinforces critical systems such as ambulance services, all to strengthen the public health system in Kono District.
A Coalition for Maternal Health Progress
The Wellbody Coalition is comprised of PIH–SL, the National Emergency Medical Services (NEMS), Lifebank, Janitri, and the Sickle Cell Carers Awareness Network (SCCAN). The coalition’s expertise and engagement is guided and overseen by the SL MOH and the Kono District Health Management Team (DHMT), who are jointly responsible for public health facility operations and improvements in Kono by supporting all levels of care delivery, and ensuring integrated referral systems throughout the care continuum. We work alongside NEMS to serve the greater population of Kono District to ensure timely and safe ambulance transport. Lifebank is a company with expertise in establishing blood banks and on-demand delivery of blood services in low resource settings. Janitri is enabling an innovative maternal health technology by equipping health facility staff with a cost-effective monitoring tool to identify high-risk pregnancies. SCCAN is a Kono based organisation striving to raise awareness about sickle cell disease, prevention, and treatment options, which is a great need throughout the District.
PIH–Sierra Leone’s Hub-and-Spoke Model
The coalition is working to ensure high quality maternal and newborn health care is accessible at all levels of the community by utilizing the PIH–SL hub-and-spoke model. The hub-and-spoke model delivers a comprehensive continuum of care — from community-level care, to primary care clinics (spokes), and to district level secondary hospitals (hubs) — heavily relying on a strong referral system to prevent delays in access to care and to rapidly assign clinical specialists to complex cases. To complement this model, PIH-SL proactively engages key stakeholders in the government and community to build capacity and sustain trust in the local health care system. By working closely with the DHMT, we have been able to engage and recruit various community leaders such as paramount chiefs, female community leaders, town speakers, marketleaders, youth leaders, and Peripheral Health Unit (PHU) Leads. By doing so, we have been able to more deeply engage with, and generate buy-in from the communities’ most distinguished and prominent counsellors, who also pledge their support to the TBA program. We plan to recruit and train 100 TBAs by June 2024, and they will be responsible for providing health promotion to pregnant and lactating mothers, generating demand, and linking to quality antenatal, labour, delivery, and postnatal care at the five “spokes”. To date, we have successfully recruited and trained 50 TBAs.

Shifting the Mindset of TBAs
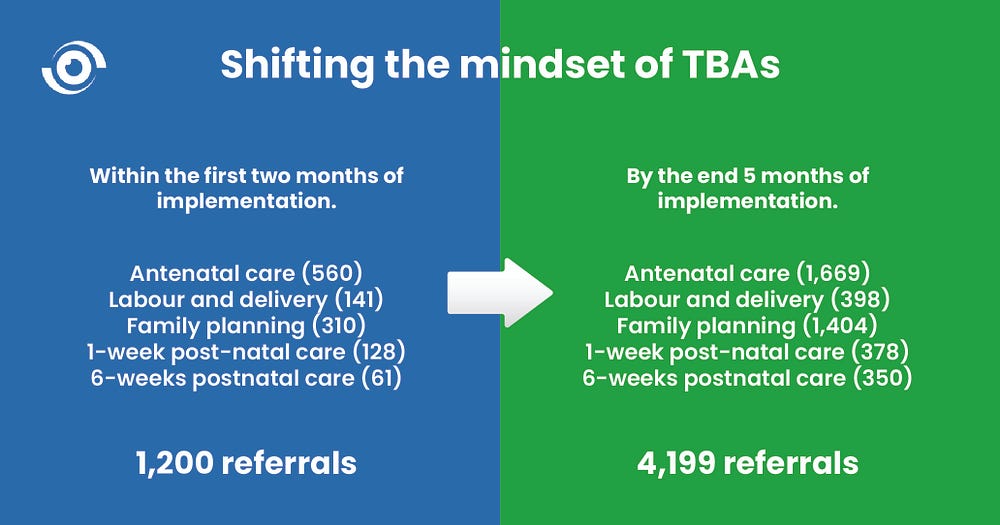
The current cadre of TBAs are already making great strides in helping to increase rates of patient referrals in Kono District. Before program implementation, TBAs brought pregnant women to facilities after the women were already in critical condition. With support from MSD for Mothers, PIH-SL has been able to invest time and resources towards building relationships with TBAs throughout key communities in Kono District. We provide localized, context-specific trainings that empower TBAs to provide referrals for safe healthcare services. Beforehand, there was no formalized referral system in place. Now, TBAs are more inclined to bring pregnant women to the clinic or hospital when they are in stable condition, proudly providing accompaniment and support, knowing that they productively contribute to the local health care system.
Within the first two months of the Wellbody Coalition’s program, supported facilities have received a total of 1,200 referrals, including those seeking antenatal care (560), labour and delivery (141), family planning (310), 1-week post-natal care (128), and 6-weeks postnatal care (61). After 5 months of implementation, the program received a total of 4,199 referrals including those seeking antenatal care (1,669), labour and delivery (398), family planning (1,404), 1-week post-natal care (378), and 6-weeks postnatal care (350). The coalition will also strive to increase community reach to 80%, establishing a system that will meet the needs of approximately 79,000 pregnant women in Kono each year, with hopes for eventual scale-up. Throughout our engagements, we keep the TBAs’ mantra of, “referral, referral, referral” top of mind.
Notably, progress has not been without its challenges. As is often the case, programmatic success produces increased patient demand which necessitates sustained investments for an increasing number of supplies, equipments, commodities, and medicines — and long-term funding remains an issue. As we embrace our collaborative and innovative approach, we will continue to support women throughout their pregnancy journeys, increase the rates of referrals for safe facility-based births, and ensure a healthier future for the mothers and newborns of Kono District. By fostering a relationship that leverages the unique skillsets and cultural insights of TBAs, the Wellbody Coalition is ensuring that the women of Kono access high-quality, safe and affordable maternal health care. Ultimately, the successful collaboration between TBAs and the formal health care system stands as a testament to our commitment to forging a more inclusive, safe, and effective future for maternal health care.
This program is supported by funding from MSD for Mothers, the company’s $650 million initiative to help create a world where no woman dies giving life. MSD for Mothers is an initiative of Merck & Co., Inc., Rahway, N.J., U.S.A.
Bios
Sabrina Charles, MPH
Sabrina Charles is the Communications Associate for Partners In Health Sierra Leone. In her role, Sabrina showcases the organization’s unique mission, values and accomplishments through storytelling. Through the remarkable human stories she tells, she advocates for a preferential option for the poor in health care. Prior to her current role, Sabrina worked with the Community Health Acceleration Partnership, as a Program Officer, she led the strategy behind grant making initiatives for birth equity programs. Sabrina has also worked as a Project Manager for Partners In Health United States advocating for health equity and justice at the local, state, and federal level. Sabrina is a native of Detroit, MI.
Billy Mawindo, MSc-SRHR, MGHD
Billy Mawindo is a values-driven leader, an experienced healthcare professional and researcher currently working as the Reproductive, Maternal, Newborn, and Child Health (RMNCH) Program Manager at Partners In Health Sierra Leone where he plays a crucial role in designing and operationalizing RMNCH programs. Billy has always been committed to making a positive impact in his community and beyond. Through his visionary leadership and tireless dedication, Billy has made a profound impact on the lives of adolescents, youth, and survivors of gender-based violence in Kono District, Sierra Leone.


