Editor’s Note: Dr. Opeyemi Adeyemi came back to Nigeria in 2015 after completing her MSc in Public Health. She started practicing in 2016. Just over a year ago, she began her residency in Community Medicine at the Olabisi Onabanjo University Teaching Hospital in Sagamu, Ogun State. When the COVID-19 outbreak came to Nigeria, Ogun State was ground zero, and Adeyemi and colleagues found themselves quickly supporting the state’s response. In this insightful interview into the life of a frontline health worker, she shares her experiences as part of the surveillance unit for the state’s only isolation centre at the time when the outbreak was just beginning. At the time of this conversation, she had been working at the centre for three weeks.
The day I heard of the first COVID-19 case in Ogun State
I was at work and we were doing some sensitisation for Lassa fever. I was like “We are not ready! We are still dealing with Lassa fever”. Amongst my colleagues, the first thing we said was, “Now it’s time for us to work”, because for public health, doctors in other areas of specialisation would say that we were not doing anything much and we were just chilling.
Generally, we were not prepared, because even during the conversations around Lassa fever, we had not had any confirmed case, only suspected cases. We were still fighting for personal protective equipment (PPEs) for Lassa fever, before COVID-19 came. We didn’t have an isolation ward then. We only had a holding bay, where we keep suspected cases until they were confirmed, so we knew we were not ready at all. Even now, our preparation level is not 100%. Preparedness is a continuous process.

My first patient
With my first patient, I had to do everything including disposing her urine and cleaning her up because I was the only one wearing PPE. Others did not have PPE, so they could not see her and get themselves exposed. Unfortunately, she passed away and then I had to wait for the result of her COVID-19 test. And then, I saw a picture of the way I was gowned in my PPE, I had one strand of hair coming out. I wasn’t a 100% covered. I panicked for about 48 hours until the results came out and it was negative! For every patient you see or every suspected case, you’re practically at risk because you don’t know what the turn of events will be. You have to ensure that you are well covered. PPE is not comfortable at all. You are practically sweating your eyeballs out; it is itchy and uncomfortable, and you still have to do your work. It’s not a sit-in PPE, so every time you come out from the ward, you have to remove it. The next time you go in again you have to re-gown. With that process, you can go in and out for up to four times, depending on how restless the patient is. Right now, it’s getting better. We are learning as cases come.
My best day at the isolation centre
Whenever I see joy in the eyes of the patient is my best day. When patients come in, it’s a panicked atmosphere because there is already a bit of stigma. Imagine a patient seeing the doctor through the eyes of PPE. They don’t really know who they’re conversing with. The patient-doctor relationship is still there, but you’re trying your best to calm the situation as much as you can and reassure them not to worry. Beautiful for me is when a patient has two negative results, gets their discharge paper, and we allow them to go home to their families. Overall, there is joy that comes with every patient’s release.
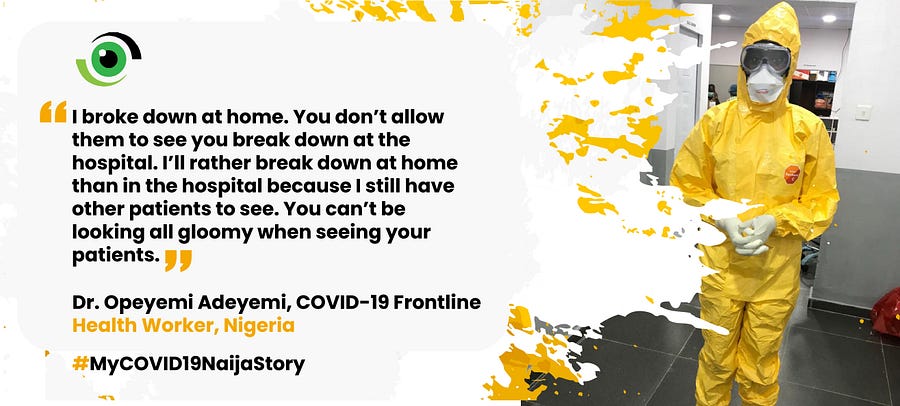
The day I broke down
I broke down the day my first patient died. I panicked a lot because I took care of everything for the patient. I emptied her urine bag. The bed was filled with blood because she was very restless, and I took care of all of that.
When I got home that day, the first person I called was my mom and she prayed with me. I called my family and I was like, “I don’t know what is going on, but my patient passed away and I’m not sure what the result is”. I broke down at home. You don’t allow them to see you break down at the hospital. I’d rather break down at home than in the hospital because I still have other patients to see. You can’t be looking all gloomy seeing your patients.
My longest day at the centre
I don’t have a day that was my longest. But my first week was the longest week. We were just two doctors; I would run the 8am-6pm shift and my colleague would run the 6pm to 8am shift. I learnt a lot in my first week. It was so busy. I wouldn’t even remember to eat. Then, there was more training for more people and things got much better. On the other hand, there’s still a bit of stigma amongst health workers. For example, other health workers that know that you are part of the COVID-19 team, do not want to come near you because of the risk of infection.
The day I thought I got exposed
The day I saw my first patient was the day I felt exposed. I had a lot of contact with my patient’s body fluids, including her blood because she removed the line I had set as she was very restless. Her blood spilled everywhere on the bed. I wasn’t prepared for that. You know the theory, but when you are there, you’re practising what you’ve been taught. It was a whole different ball game for me.
The day I stayed strong for my patient
I had to explain to a Muslim patient’s relatives that, the way their mother will be buried would be way different from the usual way they are used to. Having to explain all of that can be very daunting. For this patient, we had to put her in a body bag which is black, like a waste bag. I had to explain why we had to put their mother in that kind of bag and inform them that only four people can be at the burial, wearing PPEs, and they would have to be isolated for 14 days or while we are sure that the COVID-19 test result of the late patient was negative. Having to sit a Nigerian down is one thing. It’s another thing to sit someone who is very religious, believes in a particular way of doing things. I had to assure them that they were all going to be fine.
We have to stay strong for patients, because right now, there’s a lot of stigma around COVID-19. They don’t know what this is. It’s a lot of support and you have to keep reassuring patients that they are going to be fine, even after recovering from COVID-19.
Unfortunately, there was no training on the mental health side of COVID-19. Mental health has really been side-lined in a lot of treatments even down to palliative care and chronic diseases. A lot of times, health workers have no training on mental health. You have to use your intuition and experience to deal with several situations.
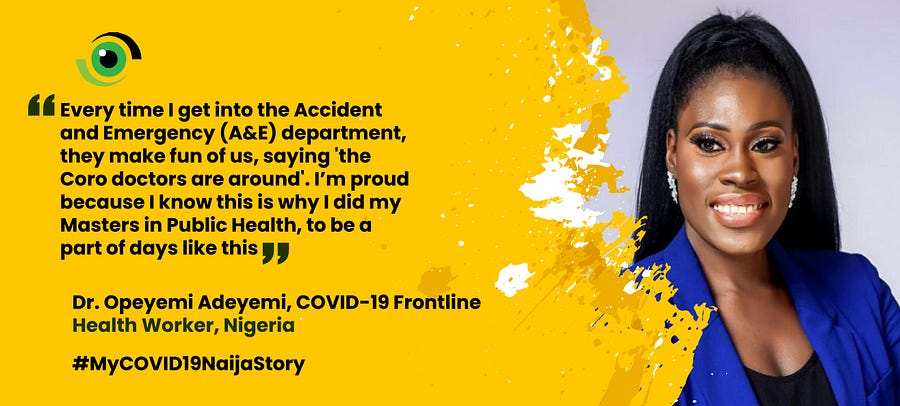
The day I was proud to be a frontline health worker
I’m very proud doing what I do. I cannot say I’m in public health, and not be excited to be part of a pandemic. I don’t know if there are any payment plans or incentives for frontline health workers. I am not working with the mindset of what I’m going to get but what I am passionate about. Whether it’s volunteering, or a paid role, it doesn’t really matter to me. I just want to be part of it. Every time I go into the A&E, they make fun of us, saying “the ‘Coro’ doctors are around”. I’m proud because I know this is why I did a master’s in public health, to be a part of days like this. Also, the moment a patient fully recovers, and you give them that discharge paper, you’re proud and happy!
The day I began to believe we can beat COVID-19
I haven’t gotten to that realisation yet. Although, we have increased our testing capacity. Nigerians are not maintaining physical distancing as they should. The earlier we test people, the more we know how many people are infected, the more we isolate and the more we reduce the amount of people exposed. Also, not as many people are as sensitised as we think. A lot of times, we just focus on people on social media, forgetting that the average Nigerian outside social media doesn’t really understand what is going on. They cannot even pronounce the name of the virus properly. We do sensitisation from time to time, go to the market, parks, schools. The last time we went to the market for sensitisation, there were quite a number of people there. It’s hard to explain to Nigerians the need for them to wash their hands and take other measures, especially for a virus that they don’t even believe.
The day that Nigeria sees her last COVID-19 case
After the incubation period of the last case, tracing all contacts that the last case had and finding that none of them have symptoms of the disease, seeing the last case would be a sigh of relief, knowing that the battle is over. It will be a joyful moment. I’ll go home, take a shower, buy chocolates, drink a bottle of wine and go to my family in Abeokuta.

Dr. Adeyemi’s Insights:
On Training
We had undergone training for Lassa Fever. Lassa Fever and COVID-19 are similar in management when it comes to personal protection. For COVID-19, we had training with the Nigeria Centre for Disease Control (NCDC) and the Ministry of Health. Doctors, nurses, attendants, down to the security team, everyone was trained. Even till now, we undergo trainings as things evolve because the pathophysiology of the virus that causes COVID-19 is still under study.
On Government Support
To an extent, we have been supported. We get free food and PPEs from them every now and then, but to be honest, they could do better. They are supportive to the extent they want to be supportive. The Federal Ministry of Health (FMOH), NCDC, the Royal Father in Sagamu, and the Rotary club have also supported us. However, we need PPEs. Every healthcare worker is on the frontline. Some even see patients without wearing PPEs. Every health worker should have access to PPEs.
On advice for the Nigerian public
Please don’t hide your symptoms. Say everything that is wrong. Don’t hide any history from health workers. Don’t expose health care workers without them knowing. Maintain physical distancing and ensure proper hand and respiratory hygiene.
We celebrate the dedicated efforts of our health workers. It goes without saying that our health security depends partly on the skills and commitment of our health workers. So, in addition to ensuring they are able to work in a conducive environment, we must all individually and collectively #TakeResponsibility to ensure that our health workers and health system is not overwhelmed. This means adhering to the key trio of public health measures, hand washing, physical distancing and wearing a face mask when going out. Only then, can we all look forwards to a day when COVID-19 is kept at bay.
All photos in this piece were used by permission. Dr. Adeyemi’s interview was transcribed and edited by Atinuke Akande and Adaobi Ezeokoli.



Well documented and proud of you
Congratulations and many thanks indeed for your work. Good account.
You and all others are deeply appreciated I can assure you.
Very impressive and proud of this young lady who is my niece. Nigeruan youths are up to the task given the chance and the right environment. We remain proud of our health workers.