Editor’s Note: Today’s piece is an OpEd from renowned Virologist and Chair of Nigeria Expert Review Committee on Poliomyelitis Eradication and Routine Immunisation, Prof. Oyewale Tomori. This World Immunisation Week, he explores Nigeria’s long road towards polio eradication and gives insights into exactly how far we still have to go before we can confidently assert that Nigeria is no longer polio-endemic.
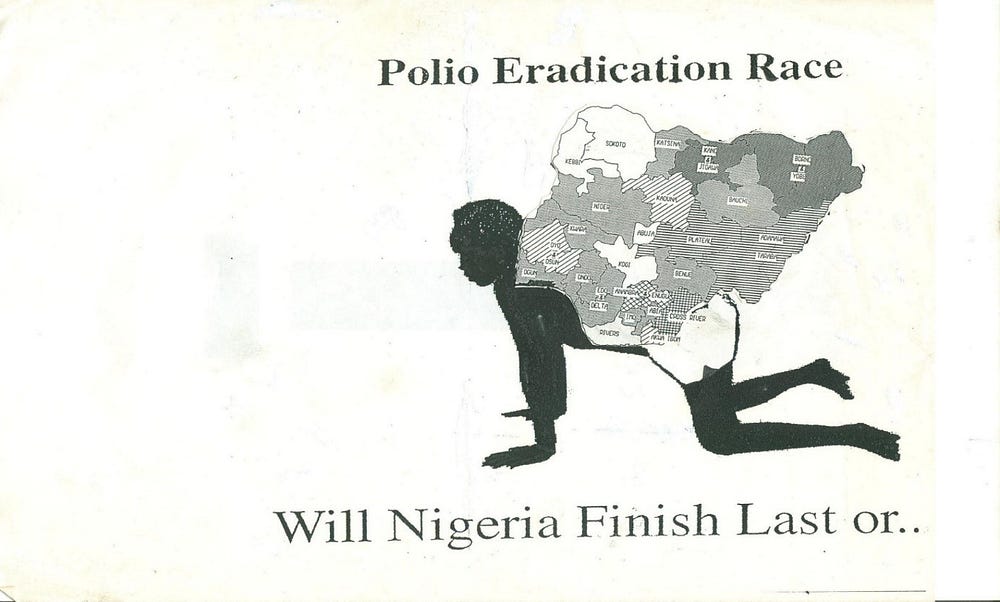
The theme for the 1995 World Health Day, on April 7, 1995, was “Target 2000 — A World Without Polio”. As part of the celebrations for the day, a lecture titled “Polio Eradication Race: Will Nigeria Finish last?”, was delivered at the Nigerian Institute for International Affairs (NIIA) Victoria Island, Lagos.
Now, 34 years later, the question is not whether Nigeria will finish last in Africa, she is already the last country in Africa to interrupt the transmission of polio, but the question now is, will she be the last to do so globally? Nigeria’s race to polio eradication has been a long and a slow obstacle race, a tortoise walk hampered by at least four self-inflicted obstacles.
First, Nigeria’s immunisation framework was erected on the sandy foundation of low coverage, a rickety edifice built with massive under-funding, uncaring attitude, casual neglect and careless abandon. Second, Nigeria began serious polio eradication activities very late — almost 20 years after the initial World Health Assembly (WHA) resolution calling for the global eradication of polio, and about 5 years to the initial eradication target of the year 2000. Third, some 16 years ago, precisely in 2003, we got diverted by the polio vaccine boycott which lasted for a little over a year, with far reaching and devastating consequences. Fourth and finally, the Boko Haram insurgency became the Achilles’ heel in Nigeria’s long and delayed finish of the polio eradication race.
While we may have gained ground over our late start and perhaps overcome the diversion of the polio vaccine boycott, the ending of the insurgency is the only thing that can see us through to the end of the race. In addition, by not addressing the issue of routine immunisation, we may somehow see off polio through unending supplementary immunisation activities but lose the big wars against other vaccine preventable diseases.

Routine Immunisation in Nigeria
The Nigerian Expanded Programme on Immunisation (EPI) was initiated in 1976 to focus on immunisation issues. It was centrally and almost autonomously managed by a national coordinator with sub-coordinators at the state and local government levels. During the military era, the selection of the coordinators was more and often based on ties rather than merit, competence, or suitability for the job. This resulted in the selection of individuals who were not best suited or qualified for the job.
Following a decade or more of lackluster performance, Nigeria reportedly attained the Universal Child Immunisation (UCI) target coverage of 80% by 1990. This was not sustained; between 1993 and 1998, immunisation coverage declined to 20–46% for DPT3. Several factors were responsible for poor performance of the EPI; The programme suffered from fickle political will and feeble financial commitment, leading to poor funding, inadequate service delivery, low social support and poor community involvement. All these, combined with poor programmatic leadership, meant that vaccines were poorly maintained in a national central store.
There were also logistic problems which ensured that vaccines were poorly distributed or not at all. With vaccine stock outs, and unavailability of syringes and needles in the few health facilities conducting routine immunisation services, millions of Nigerian children were unvaccinated. To stem the decline and recognizing that maintaining high immunisation coverage is a vital disease control strategy, the federal government, in 1997, restructured the EPI, renaming it the National Program for Immunization (NPI). Ten years later, following the Federal Government Health Sector Reform, the NPI was merged with the National Primary Health Care Development Agency (NPHCDA) in May 2007.
The change in name did little to improve immunisation coverage in Nigeria. The 10 years of NPI could well be described as the annus horribilis years for the children of Nigeria, and the annus mirabilis years for others who reportedly fed fat and voraciously, on funds meant to protect Nigerian children from the ravages of preventable diseases. The damage done to routine immunisation in the NPI years continues to be felt even today. According to the Nigeria MICS/ NICS 2016–2017, Nigeria attained the status of the country with the highest number of under-immunised children in the world (about 4.5 million). The country is also home to the deepest inequities in immunisation, both between geographic regions (e.g. coverage in Sokoto: 3%; Lagos: 80%), and between income quintiles (73% difference in coverage between lowest and highest quintile).
Nigeria’s Polio Eradication Initiative
It was in 1988, at the 41st World Health Assembly, that the landmark resolution (WHA 41.28) for the worldwide eradication of polio by the year 2000 was adopted. The target has been missed more than once. Nigeria did not seriously begin polio eradication activities until about 1996, by which time 15 African countries had successfully interrupted the transmission of polio and would have been declared free of polio but for Nigeria and 30 other African countries where polio transmission was at different levels of intensity. Of the 1,949 polio cases reported in Africa in 1996, Nigeria alone accounted for 942 or 48.3%. Seven years later, in 2003, 30 African countries had successfully interrupted polio transmission, that is reporting zero polio cases, while Nigeria reported 782 (83.7%) of the 934 polio cases reported in Africa.
The Polio vaccine boycott
The year 2003 was also the year that political, religious and academic leaders in Kano, Zamfara, and Kaduna states brought the immunisation campaign to a halt by calling on parents to reject the polio vaccine, and not allow their children to be vaccinated. A spokesman for the governor of Kano, was quoted as saying, “…since September 11, (2003), the Muslim world is beginning to be suspicious of any move from the Western world… Our people have become really concerned about the polio vaccine.” Another leader of the Supreme Council for Sharia in Nigeria (SCSN), is quoted as saying that polio vaccines were “corrupted and tainted by evildoers from America and their Western allies.” He went on to say: “…. we believe that modern-day Hitlers have deliberately adulterated the oral polio vaccines with anti-fertility drugs and…viruses which are known to cause HIV and AIDS.”
This 13-month boycott, reminiscent of some of the misinformation and boycott around MMR in some other countries, was a major setback for polio eradication in Nigeria, with long lasting repercussions in and outside Nigeria. Nigeria became an exporter of polio virus to other countries. In the year of the boycott, Nigeria reported 355 polio cases. The following year, 2004, the number of polio cases reported by Nigeria was 782, more than double the figures for 2003. In 2005, Nigeria’s polio cases had ballooned to 833. Two years after the resumption of polio vaccination in the boycotting states, in 2006, the number of polio cases in Nigeria peaked at 1,144 cases, an average of almost 18 cases per day!
In other West African countries, new cases of polio originating and exported from Nigeria were reported in Benin, Burkina Faso, Cameroon, Chad, Cote d’Ivoire, Ghana, and Togo. These countries were previously free of polio. In 2005, Indonesia reported 4 cases of wild polio. Genetic analysis of the polio isolates traced the pathway of exportation from Nigeria to Chad to Sudan to Saudi Arabia to Indonesia.
“Don’t continue being a risk” — Unflattering WHA attention
The number of polio cases reported in Nigeria, dropped from the 1,144 cases in 2006 to 356 in 2007, and increased to 866 cases in 2008. That was the year Nigeria drew unflattering attention at the WHA. The Assembly came out with a resolution calling on Nigeria not to continue to be a risk to the world urging the country to reduce the risk of international spread of poliovirus by quickly stopping the outbreak in northern Nigeria. Obviously stung by the global rebuke, Nigeria got her act together and appointed a credible and competent CEO, Dr Pate, to run the NPHCDA. Soon after, there was a steady decline in the number of polio cases from 543 in 2009 to 130 in 2012. The number of polio cases had by 2014 dropped to 36, and Nigeria was looking forward to being declared polio free by 2017.
Boko Haram’s intensified insurgency
Nigeria’s hopes of attaining polio free status was dashed by the intensified activities of the Boko Haram group, when four new cases of polio were reported in July and August 2016, in residents of Jere, Gwoza and Monguno LGAs of Borno State, areas newly liberated from Boko Haram. Genetic analysis of the polio isolates confirmed that the viruses had been circulating for between 4–5 years in the inaccessible areas under Boko Haram occupation. These new findings again brought unfavourable attention to Nigeria, making the WHO Africa Regional Committee at its 66th session in August 2016, declare the Nigerian wild polio isolations a sub-regional public health emergency for member states of the Lake Chad basin.
Since August 2016, Nigeria has not reported any case of wild polio in any of the accessible areas of Nigeria. Extra and innovative efforts are being made to reach populations in partially and totally inaccessible parts of Borno state. It is now estimated that less than 100,000 children are trapped in the inaccessible areas. By August 2019, if no wild polio virus is detected, Nigeria would have been polio-free for three years. After due consideration by the African Regional Certification Committee, of our immunisation coverage, level of AFP surveillance and existing situation in the inaccessible areas under Boko Haram occupation, the country may be considered as having finally achieved the status of interrupting wild polio transmission for the first time. There is a place for cautious optimism that by the end of 2019, Nigeria may finally be elevated to the status of a non-polio endemic country.
However, it is too early to start celebrating or begin a countdown. For two years between July 2014 and July 2016, Nigeria did not report any wild polio case, until new cases were detected among residents of recently liberated LGAs previously under Boko Haram control. We still have some areas, though largely reduced, of the country that are inaccessible for public health intervention, including polio vaccination and disease surveillance activities. Until all areas of Nigeria are accessible, there will always be some degree of reservation to asserting with full confidence that Nigeria is truly polio free.
While it is true that no wild poliovirus has been detected in Nigeria for more than two years, and no international spread of polio from Nigeria for more than four years, there are ongoing outbreaks of cVDPV2, which indicates the vulnerability to poliovirus infection in many parts of the country, including areas not previously considered at high risk of polio, such as Kwara State. In addition, Nigeria continues to have difficulties in controlling the protracted cVDPV outbreaks. Routine immunisation in Nigeria remains weak as there are still some surveillance gaps. There is still a lack of access to certain parts of the country. Experience has shown that the upsurge of polio cases in Nigeria usually follow changes in leadership of the NPHCDA, and election years when funds reportedly get diverted to political, rather than immunisation campaigns.
In 2016, we were “this close” to achieving non-polio endemic status, but missed the goal with detection of wild poliovirus in residents previously living in areas under Boko Haram influence. The current situation should caution us not to celebrate too early or begin a countdown to polio eradication in Nigeria. We are now in extra time of the second and possibly final half of the polio eradication race. We must be vigilant not to concede a late own goal before the race ends.
BIO: Prof. Oyewale Tomori is the immediate past President of the Nigerian Academy of Science with experience in virology, disease prevention and control. He was at the University of Ibadan from 1971 to 1994. He later served as the pioneer Vice Chancellor of the Redeemer’s University in Nigeria from 2004 to 2011. From 1994 to 2004, he was the virologist for the World Health Organization (WHO)’s Africa Region, establishing the African Regional Polio Laboratory Network. In 1981, he was recognized by the U.S. Centers for Disease Control and Prevention (CDC) for contributions to Lassa fever research. He has authored/co-authored over 150 scientific publications. Prof. Tomori has served or continues to serve on numerous advisory committees, including: (nationally) — Chair, Lassa Fever Steering Committee, National Laboratory Technical Working Group, Expert Working Group on Polio Eradication and Routine Immunization, etc, and (internationally)- WHO SAGE, WHO Africa Regional Polio Certification Committee, WHO Group of Experts on Yellow Fever Disease, Chairman WHO Yellow Fever Emergency Committee on International Health Regulations, GAVI Board, Vice Chair of U.S. National Academy of Medicine Global Health Risk Framework Commission, and World Bank Interagency Working Group on Financing Preparedness and Response. He is an international member of the U.S. National Academy of Medicine and currently Chair, Board Biovaccines Nigeria Ltd.


Congratulations, Nigeria Health Watch, on this excellent and insightful outing. I appreciate revered Prof Oye Tomori’s depth in relaying our country’s long journey to polio elimination. I therefore fully identify with his admonition to all stakeholders on the issue.
As a matter of fact, I’m one of those who believe that the time has come for our federal State governments to truly design context-specific approaches to ensuring effective and sustainable routine immunisation practice for better coverage for Nigeria. A one-style design/framework will most likely deepen the existing inequity of access for most parts of low population density North and areas of difficult and high-cost access in the creeks of Niger Delta.
Nice piece! Congratulations again.
Congratulations to Professor Tomori and all Nigerian professionals in reaching this milestone. Lessons learned in this long campaign was that round pegs must be placed in round holes. Leadership must be a continuum in all public health efforts to contain menacing diseases. The Kano rejection of polio vaccine in 2005 was primarily a communication gap issue which was mishandled and exploited by politicians and self serving ‘religious leaders ‘