By Michael Atima and Bunmi Oyebanji Obot (Lead Writers)
It is a little-known fact that 5–10% of pregnancies in Nigeria are complicated by hypertension issues. Despite the significant burden of maternal mortality and morbidity (MMM), there hasn’t been sufficient focus on how noncommunicable diseases (NCDs) affect women of reproductive age and their risk factors.
The Federal Ministry of Health (FMoH) has demonstrated its commitment to addressing NCDs by establishing an NCDs division, developing a national noncommunicable diseases multi-sectorial plan (2019–2025), and incorporating diabetes and hypertension coverage into the Basic Minimum Package of Health Services (BMPHS) through the Basic Health Care Provision Fund (BHCPF). Despite the substantial burden of NCD-related ‘indirect causes’ of maternal mortality and morbidity among women of reproductive age, there has been little attention paid to the unique vulnerabilities of women of reproductive age (WRA) with NCDs and associated risk factors. A global burden of NCDs contributing to maternal morbidity and mortality must be addressed through a systemic approach to improving maternal health.
RICOM3 — piloting the ‘Quality of Care’ model
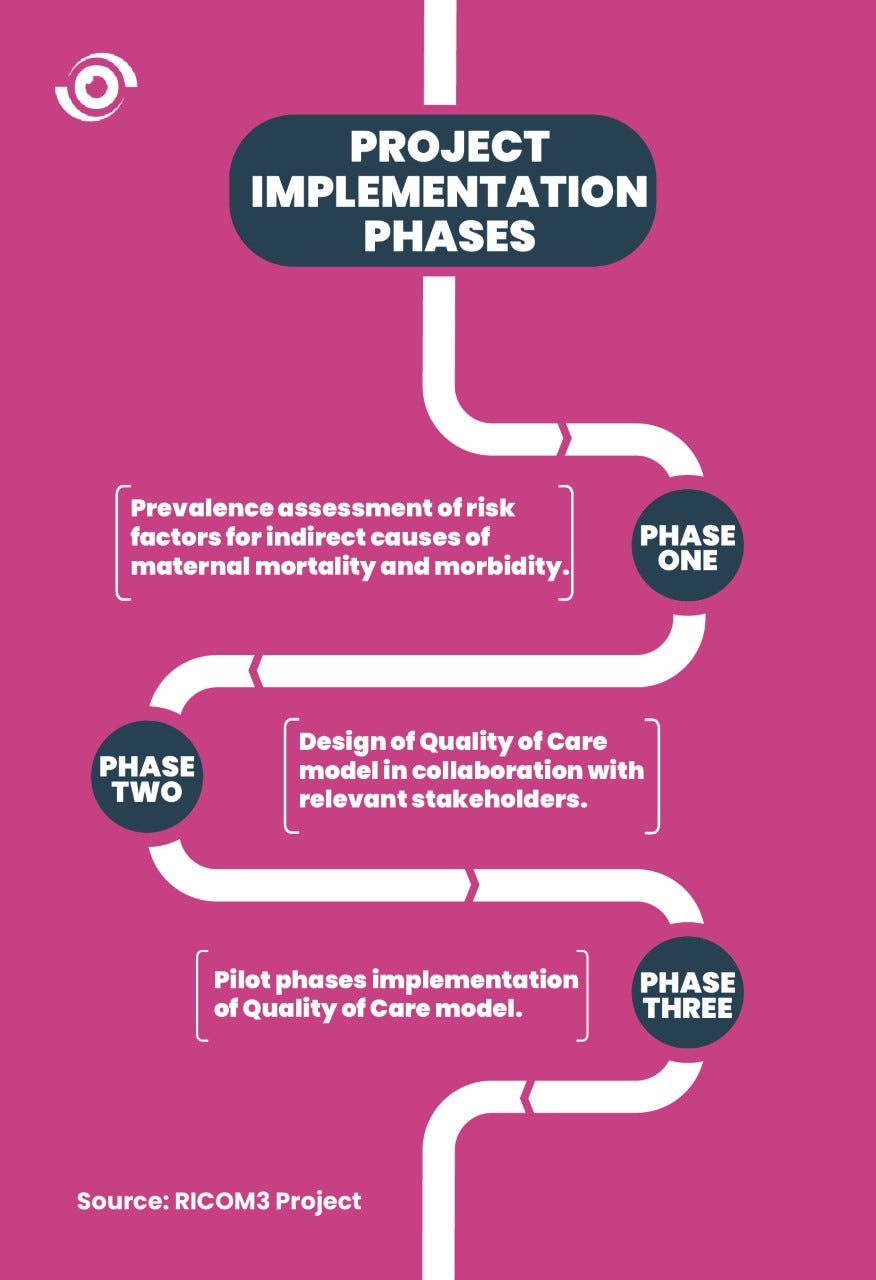
The ‘Reducing Indirect Causes of Maternal Mortality and Morbidity’ (RICOM3) project began in 2019 and was concluded in 2022. It was developed with support from MSD for Mothers and implemented by a consortium comprised of Jhpiego, mDoc and Health Strategy and Delivery Foundation (HSDF). The RICOM3 project aimed to reduce morbidity and mortality among women of reproductive age in Nigeria by implementing an innovative and integrated Quality of Care (QoC) model at the subnational level. The QoC model was created as a woman-centered care model that incorporates elements of self-care, using digital technology and quality improvement (strengthening the health facility’s capacity) to increase access to screening and management of hypertension, diabetes mellitus, anemia, and obesity at maternal health care touch points and reduce their contributions to indirect causes of maternal mortality.
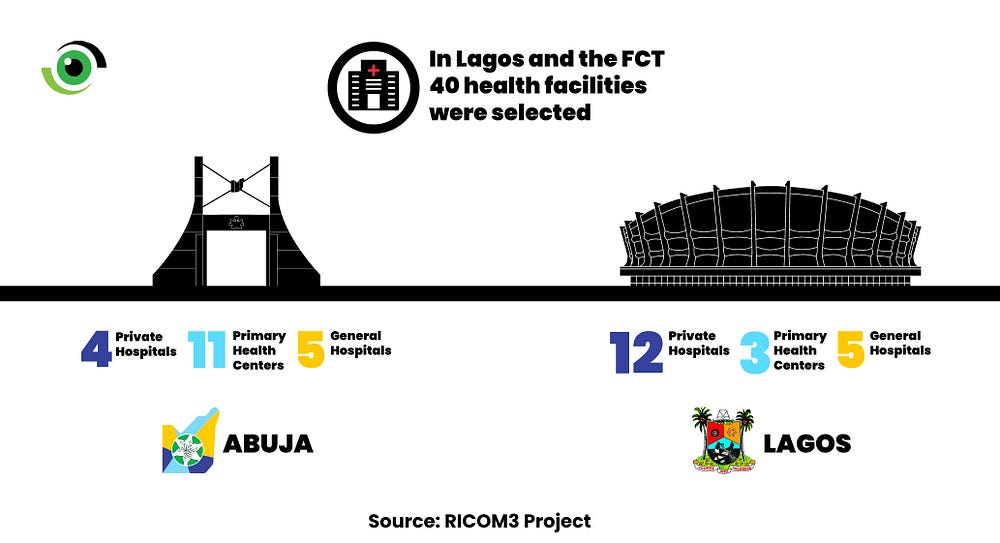
The project was implemented in two local government areas, each, in Lagos State and the Federal Capital Territory (FCT): Alimosho and Ikorodu in Lagos State, and the Bwari and Abuja Municipal Area Councils, in the FCT. In both states, 40 health facilities were selected, including primary, secondary and private hospitals. In the FCT, there were four private hospitals, 11 basic health centres, and five general hospitals, while Lagos had 12 primary health centers, three general hospitals, and five private hospitals.
A preliminary assessment found that a high knowledge gap in identifying and understanding hypertension symptoms for women, health workers’ poor knowledge about quality of care, and provision of low-quality services were all contributing factors to maternal deaths.
The parts that make up the body
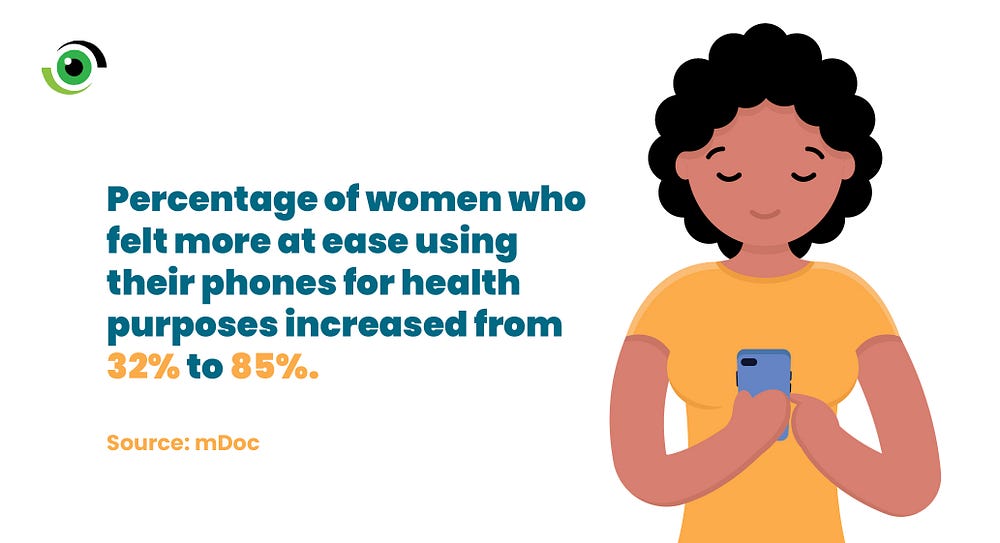
The consortium committed to addressing these issues in various capacities. mDoc used its digital health platform to educate pregnant women throughout the course of their pregnancy. The introduction of the CompleteHealth™ platform provided virtual guidance in self-care and lifestyle modification. A multidisciplinary self-care team and health coaches were made available for nutrition, emotional wellness, and fitness through one-on-one coaching calls, texting, and digitally tailored action plans. SMS and Unstructured Supplementary Service Data (USSD) were supported by the platform for users with low-end phones. Online individual and group digital platforms, peer-to-peer learning was promoted, health promotion messages were exchanged, and questions were answered around the clock. It also included infographics and instructional tools, such as exercise workout videos and information on dealing with anxiety and depression.

HSDF focused on the cost implications of quality care versus the absence of quality care to the government, providing a bird’s-eye view of the financial implications of the endeavor and a report on the savings provided. Jhpiego led the integration of NCDs across the maternal health care continuum, empowering health care workers in the selected health facilities to provide a more integrated and holistic level of care, resulting in better quality maternal health outcomes.
The results so far
The RICOM3 project discovered that women have better conversations with their health coaches and nurses after increased knowledge about self-care during pregnancy and improved capacity of health care workers, resulting in more efficient and effective service delivery. The selected health facilities also reported improved documentation, a decrease in the number of maternal deaths observed across the project states, and cost savings as a result of the QoC model’s expansion into Health Maintenance Organisations (HMOs.
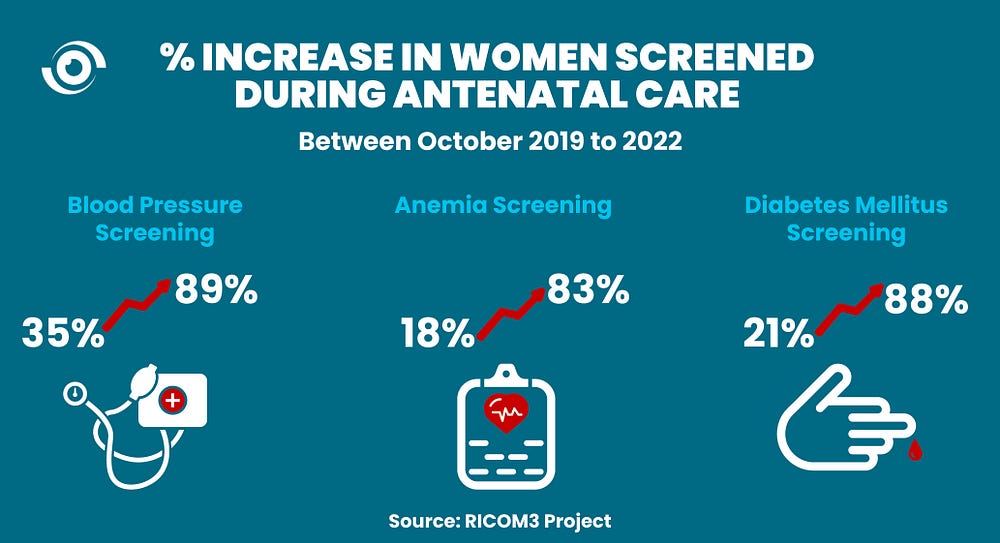
The percentage of women reporting self-confidence in managing their health increased by 48% on average in both the FCT and Lagos State. According to Jhpiego’s endline survey, 728 health care workers from the 40 supported health facilities participated in the capacity building program. The screening of women attending ANC in these facilities for blood pressure increased from 35% in October 2019 to 89% in October 2022, anemia screening — 18% to 83% and screening for diabetes mellitus — 21% to 88% in the same period. HSDF also investigated options to support the long-term viability of the integrated QoC model. HSDF enlisted a top private HMO in Nigeria, and they agreed to incorporate the QoC model into the benefit packages of women of reproductive age (WRA).
Dr. Oludara Folashade, Director of Family Health and Nutrition, Lagos State Ministry of Health, reiterated the enormous impact of the RICOM3 project in the state, and how critical the implementation improved maternal health outcomes in the selected facilities, at the project’s conclusion. She revealed the state’s commitment to sustaining the project’s gains made possible by the successfully implemented QoC model.
A few of the many successes
Mrs. Olumide, a 33-year-old mother of one who was 37 weeks pregnant and had a blood pressure of 140/90, was concerned by her doctor’s recommendation that she have a caesarean section (C-section) rather than a vaginal birth. Her main concerns were the stigma associated with having a C-section and what her family and friends would think. Her health coach offered her emotional support as well as advice on how to change her lifestyle to lower her blood pressure and be more active while pregnant. Mrs. Olumide’s blood pressure has dropped to 120/70 mmHg after working with her coach to implement lifestyle changes. She is still grateful for and delighted with the programme’s contribution to her shift in attitude toward her health and well-being.

Another beneficiary was scheduled for IVF delivery with blood pressure 210/140mmHg, weight 60kg, height 1.65, BMI 25.7, PCV 36%, and RBS 7.1. The nurses gave her health advice and immediately referred her to the consultant, who saw her and put her on the proper blood pressure medications. She was closely monitored and given anti-hypertensive medication until the C-Section of a live male newborn. Before being sent home, her blood pressure was stabilised at 120/70mmHg. She went to postnatal care three times. The infant received his immunisations as directed, and both mother and child are doing well.
Learnings from RICOM3 and recommendations for policy and action
Combating NCDs in reproductive-age women is critical to lowering Nigeria’s maternal mortality ratio, which is currently estimated at 512 per 100,000 live births.
- The support of key government stakeholders is critical to ensuring that the QoC model becomes the standard for the majority of domestic facilities.
- More funding is required for such interventions to be integrated with other ongoing programmes. While NCD screening has been successfully integrated into the Maternal Newborn and Child Health Week programme, the RICOM3 activities cannot be implemented in all health facilities due to a lack of funding. Capacity building is required to support advocacy for limited resources.
- The RICOM3 project demonstrated the importance of digital health in increasing access to maternal health services. An integrated QoC model or approach for WRA living with or at risk of NCDs must include digital self-care support.
The benefits of the RICOM3 project should be sustained and replicated across the country. As part of the project’s exit strategy, the consortium created a sustainability plan. Future programmes should build on these discoveries to contribute to creating a world where no woman dies while giving birth.


