Nigeria, like many other countries, has been experiencing a health worker migration crisis which is posing a challenge to achieving universal health coverage (UHC) and meeting the Sustainable Development Goal (SDG) targets.
Migration is a natural human occurrence, and low- and middle-income (LMICs) countries have benefitted from health worker migration through the receipt of remittances, in addition to having a pool of skilled health workers who may return home and share their expertise and knowledge.
Speaking on the panel, “Private Sector Partnerships and Collaboration to Sustain the Diaspora “Brain Gain, during the 2023 Future of Health Conference themed, “The Private Sector as a Catalyst for a Resilient Health System”, Professor Cheluchi Onyemelukwe, Managing Partner, Health Ethics and Law Consulting acknowledged that emigration can be inevitable. “We recognise that people are going to leave regardless of how wonderful things are. People leave the United States (US) to other places; people leave Canada to the US and so on,” she however advocated for managed migration which involves implementing policies and strategies that facilitate migration in a manner that benefits both the migrants and the society.
Sustaining the #BrainGain4Naija
Nigeria Health Watch has consistently advocated for harnessing the diaspora’s potential to reverse Nigeria’s medical brain drain. The 2018 Future of Health Conference, “The Diaspora as Nigeria’s Brain Gain” featured Nigerian healthcare professionals in the diaspora who had returned to add value to Nigeria’s health sector. Speakers at the conference — some had returned fully, others visited periodically and regularly — shared their experiences and discussed ways to create a more supportive environment for returning professionals.
The panellists during the session, Njide Ndili, Country Director, PharmAccess, Nigeria, Nigeria, Ejim Egba Clement, President, Nigerian Medical Students Association (NiMSA), Dr. Benjamin Anyanwu, Executive Medical Director, Regions Healthcare Hospitals and Specialist Clinics and Prof Cheluchi Onyemelukwe, Managing Partner, Health Ethics and Law Consulting, discussed the critical role of private-public partnerships (PPP), innovative strategies for healthcare financing, and the need for comprehensive policies that prioritise the retention and engagement of healthcare professionals, particularly those from the diaspora.
Start private, grow public
Njide Ndili discussed the many opportunities for skilled healthcare professionals in the diaspora who are contemplating returning to Nigeria. “When you go around talking to quite a few of the diasporans, they are very interested to come back to Nigeria and to contribute but they don’t know how…So, what we are doing is engaging them and showing them opportunities in areas where they can come and invest and be part of the rebuilding of our healthcare systems”.
She discussed the significant role of private sector engagement, the need for public-private integration and stressed the importance of understanding Nigeria’s complex healthcare ecosystem. Public-private integration involves a deeper and more comprehensive merging of public and private sectors in service delivery, beyond forging partnership. Details are captured in the Nigeria Health Sector Market Study Report which provides insight into the opportunities in the health sector and highlights market opportunity case studies on Primary Health Centre (PHC) revitalisation, telemedicine and vaccine production.

Ndili emphasised the critical relationship between the private sector’s innovative potential and the government’s role in enabling scalable and sustainable health interventions. “Innovation starts in the private sector, but you cannot scale and sustain if you don’t involve the government”. Such partnerships can help produce “pull” factors in the form of constituting policies that would incentivise Nigerian healthcare professionals in the diaspora to return, and enable their seamless integration.
A conducive environment for growth and development
Mr Ejim Egba Clement discussed the abundant opportunities for the private sector to collaborate and partner with medical students which would help foster innovation, encourage their contributions to the local healthcare landscape and ultimately, a sense of patriotism. He highlighted the work being done by the Nigerian Medical Students Association (NIMSA) to promote research and innovation in the health sector. “Recently, I was privileged to sign an MoU with Future African Scientists. We are currently trying to see how we can establish research hubs across the six geopolitical zones in Nigeria”. He added that, once established, these hubs will provide medical students an opportunity to start research studies, post medical school.

Clement highlighted a health innovation challenge launched in collaboration with the Ooni of Ife’s Royal African Foundation. The objective was to encourage medical students across Africa to identify health-related problems in their community and propose viable solutions.
Drawing attention to the numerous challenges faced by medical students in Nigeria, particularly the “drastic fee increases in some universities, reaching up to a 1000% for medical students,” Clement proposed the establishment of a “fund pool” specifically for medical students. Additionally, he suggested implementing a “bonding programme which is already in practice in some northern states in Nigeria. Under this arrangement, students receive monthly stipends and after graduation, they are expected to return to the state and serve for a designated period.” He urged the private sector to adopt this strategy, in addition to offering soft loans, grants, and sponsorship for medical students.
“We came down to Nigeria to establish a neuroscience institute in Owerri, Imo state.”
At “The Diaspora as Nigeria’s Brain Gain” conference in 2018, health professionals, who had returned to Nigeria, unanimously agreed that the decision to relocate to Nigeria was not for the “fainthearted”. However, they also acknowledged that there was clear evidence that the Nigerian health system had benefitted from their expertise and skills.
Dr. Benjamin Anyanwu echoed this sentiment as he recounted his journey leaving Nigeria for the United States after medical school and returning to establish a successful multi-specialty hospital. He stressed the importance of creating an enabling environment for professionals to return and contribute to the health system. “We came down to Nigeria to establish a neuroscience institute in Owerri, Imo state. It was a purpose-built hospital but with ideas to expand we started doing the things we knew best to do, which was neuroscience and neurosurgery,” he said, adding that his success lay in being able to collaborate with his colleagues in the diaspora and in Nigeria.
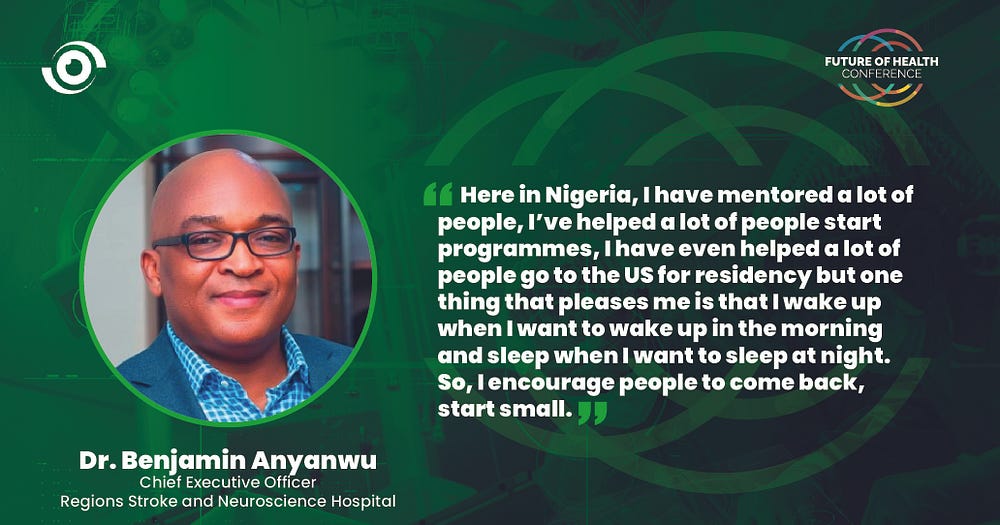
Beyond creating an enabling environment for people to return, there is also the need to create an enabling environment for people to stay. He is among the many doctors from the diaspora who returned home and are making a significant impact, and from his wealth of experience he offered valuable insights for anyone contemplating a similar feat: “the opportunities are here, come back when the ovation is loudest, start with what you have, start little, and grow big, leverage collective expertise, collaborate with professionals from abroad and local health providers for knowledge exchange and mutual support”
Dr. Anyanwu also posed a thought-provoking question that is crucial for Nigeria to fully tap into the potential of reversing the brain drain: “How can we work with the government to create a soft landing for health workers who want to come back?”
Harnessing the power of policy coherence and story telling
To effectively reverse the brain drain in Nigeria’s health sector, Professor Onyemelukwe advocated for a comprehensive and strategic approach that encompasses policy coherence, bilateral agreements, holistic incentives, and storytelling to foster an environment conducive to the return and contribution of health professionals.

Nigeria is on the World Health Organization (WHO) health workforce support and safeguards list 2023. These are countries with a density of doctors, nurses and midwives below the global median (49 per 10 000 population); and a UHC service coverage index less than 55. Prof Onyemelukwe believes that this represents an opportunity to address the underlying issues and tackle critical challenges such as fair recruitment practices, financial compensation for the training and development of healthcare professionals, and mechanisms for knowledge sharing and collaboration. “Basically, what it means is that we are training healthcare professionals for the world and it’s not as if we have enough for ourselves,” she said.
Nigeria has a National Diaspora Policy in place, which aims to recognise and harness the diapora’s potential, empower them to contribute effectively, and protect their rights and welfare. However, according to Prof Onyemelukwe who contributed to the policy’s drafting, “Since that time, some of the conversations that we have had, for example, around tax incentive and so on, have not yet yielded any fruit”. She also disclosed that a policy for health worker migration is under development and advocated for the involvement of all relevant stakeholders to ensure a comprehensive policy.
Prof Onyemelukwe in addition underscored the power of storytelling as a catalyst for change. She emphasised that positive examples and successful partnerships, alongside how a coherent approach to policy formulation and implementation can help reshape the narrative and foster a conducive environment for the return and active engagement of health professionals in the diaspora.



