A shortage of well trained, and motivated Human Resources for Health (HRH) and inadequate funding are some of the challenges confronting Nigeria’s Primary Health Care (PHC) system. Against this backdrop, in June 2022, Nigeria Health Watch organised a policy dialogue on the theme “Strengthening Human Resources for Health and Achieving Sustainable Financing for Primary Health Care” in Kano State.
Kano State has, over the years, implemented some significant initiatives that have boosted the state’s primary healthcare system. Having allocated up to 15% of its budget to health since 2020, the state has also deployed innovative funding mechanisms for health among which include, the State Health Trust Fund and the Kano State Contributory Health Care Management Agency (KSCHMA). In addition, Kano State is one of the states implementing the Minimum Service Package of care in PHCs in the country.
The state therefore provided the perfect backdrop to discuss the key issues around HRH and health financing at the PHC level, the standards and requirements for primary healthcare service delivery, particularly for human resources and financing, and to explore the benefits of leveraging the private sector for health financing and HRH in the delivery of PHC services.

Factors influencing the HRH gap in PHCs
The HRH gap in PHCs across Nigeria is a product of multiple challenges, one of which is the lack of adequate training for health workers. Dr. Aminu Ibrahim Tsanyawa, Kano State Commissioner for Health said several primary health facilities in the state are grappling with the challenge of poorly trained health workers, as many workers in the primary healthcare system in the state do not have the required qualifications.

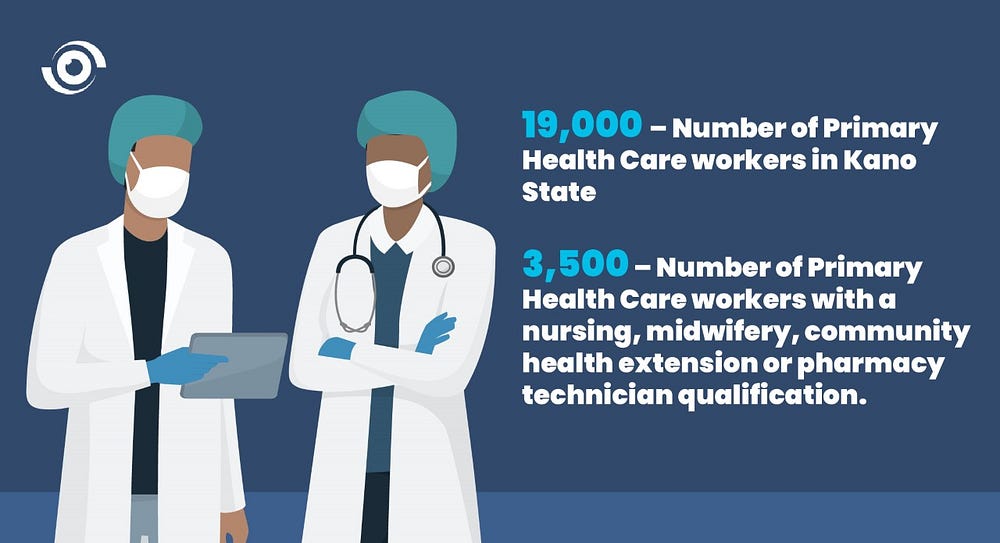
According to Dr. Tijjani Hussaini, Executive Secretary, Kano State Primary Health Care Management Board (KSPHCMB), there are over 19,000 primary healthcare workers in Kano State, 9,000 of whom are frontline health workers; and only a little over 3,500 have either a nursing, midwifery, community health extension or pharmacy technician qualification. The rest, he said, have environmental health science or medical record qualifications. This has created human resources gaps in the PHCs, and ultimately affected the quality of services the facilities deliver
Dr. Hussaini also described the unwillingness of some health workers to be deployed to PHCs in rural and hard-to-reach communities as a driver of the HRH shortage in rural health facilities. This, he said, is mostly due to factors such as distance from family, poor access roads, lack of basic amenities or poorly equipped PHCs in the communities they have been posted to. This is often why trained health workers are concentrated in towns and urban communities, he added.
State Health Trust Fund, BHCPF and KSCHMA providing vital funding
The purpose of the Basic Health Care Provision Fund (BHCPF) and state health insurance schemes such as KSCHMA, is to provide the much-needed funding and support to improve service delivery at PHC level. Dr Hussaini revealed that there are currently 381 PHCs under the BHCPF in Kano State. These PHCs use the capitation they receive to fund critical interventions, including refurbishment of essential infrastructure and equipment, procurement of essential medicines and engagement of ad-hoc healthcare workers. In addition, according to Dr. Abdullahi Sa’ad, Director of Programmes, KSCHMA, every month, over 300 PHCs in the state receive capitation from the agency, which enables them to invest in critical areas of need in the facilities.
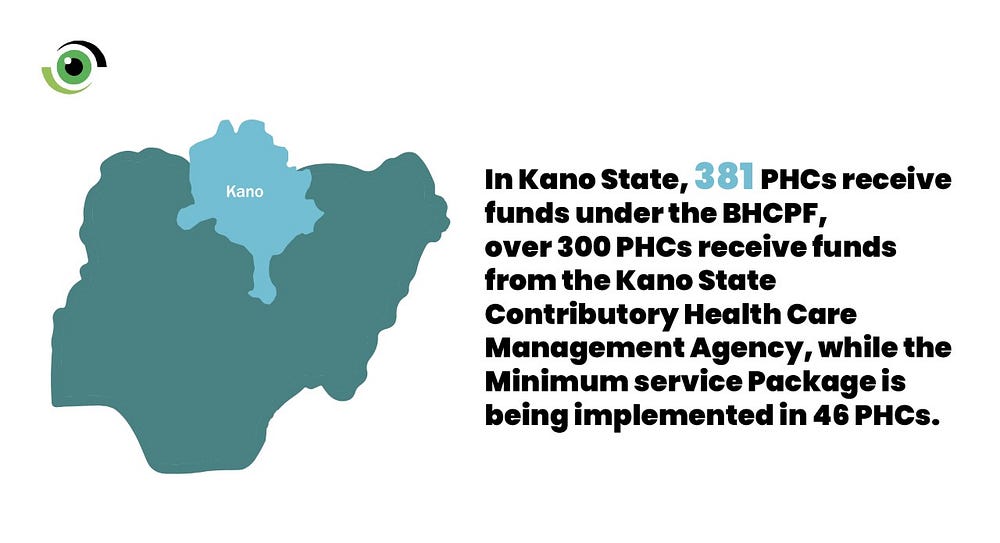
However, proper, and prudent management of available resources was a challenge, Dr, Tsanyawa said. As a result, Kano State began the implementation of the Minimum service Package (MSP) in 2019, where amongst other things, staff of selected health facilities are trained in resource mobilisation and management. So far, the MSP is being implemented in 46 primary health facilities in the state, all of which receive capitation from the BHCPF and KSCHMA and funding support from the Kano State Health Trust Fund (KSHTF). According to Dr. Ashiru Abubakar, Senior Associate at Clinton Health Access Initiative (CHAI), a partner supporting the MSP implementation in the state, these 46 health facilities have utilised the resources to engage more staff, build and equip laboratories, maternity wards, delivery rooms and dispensaries.

Bridging the service delivery gap
Several private health care delivery models have helped bridge the health service provision gap in Nigeria. One of such models, is integratE, implemented by the Society for Family Health (SFH) and PharmAccess Foundation and co-funded by the Bill & Melinda Gates Foundation and MSD for Mothers in some states, including Kano State. According to Dayyabu Yusuf, Regional Manager Northwest, SFH, the HRH challenge in PHCs is one of the reasons for the implementation of the integratE project, under which community pharmacists and patent and proprietary medicine vendors (PPMVs) are trained to deliver a wide range of PHC services, including family planning. This, according to Yusuf is helping to augment the shortfalls and shortages in service delivery as community members have options of accessing select services such as family planning from the pharmacies and PPMV stores.
Key takeaways
The conversations were rich and scintillating as insights, knowledge and recommendations shared by the delegates concluded with the following key takeaways;
- Community Based Health Insurance Schemes (CBHIS) can improve equitable access to healthcare for Nigerians in the informal sector. Paul Hogan, the Executive Vice President of EHA Clinics, cited the REACH Programme implemented by EHA Clinics in Kano state as a proven concept.
- There is a need to address the skills gaps in HRH by leveraging the existing Task Shifting and Task Sharing policy like the KSPHCMB did in 2017, where health workers with minimal or no health training were trained to provide skilled services especially in the areas of maternal, newborn and child health.
- Mitigate the HRH shortage by adopting the home-grown health worker scheme where young girls and boys are recruited and sent to health training institutions where they acquire the necessary skills and upon graduation, are deployed back to their communities to fill the HRH gaps. The concept was demonstrated by Women for Health in a programme designed to bridge the HRH gap in PHCs.
- Leverage on private sector models for health financing and HRH in the delivery of PHC services. Programmes like integratE leveraged on community pharmacies and PPMV stores to provide services to complement primary health care facilities.
- Address health worker unwillingness to be deployed to rural and hard-to-reach areas by ensuring that all PHCs around the country are equipped with the vital infrastructure and social amenities to enable the deployment of health workers to communities facing health worker shortages.
As outlined in the PHC summit organised by the Federal Ministry of Health in March 2022, increasing, and improving the quality of HRH — which cannot be achieved without adequate financing — is the key to achieving the transformative plan of improving and expanding primary health care in Nigeria. It is imperative that the discussions at the PHC Policy dialogue are translated into action by policy makers, especially at the sub-national level, to ensure the PHCs are functional and able to provide quality health care services to Nigerians.


