We have heard the statistics countless times.
Nigeria accounts for nearly 20% of global maternal deaths according to the World Health Organisation (WHO). According to the Nigeria Demographic Health Survey 2018, only a mere 39% of live births occur in health facilities, with 61% of births taking place outside of a health facility. According to the United Nations Population Fund (UNFPA), Nigeria loses $1.5 billion yearly to maternal deaths.
In January 2019, a consortium consisting of Africare, Nigeria Health Watch and EpiAFRIC was established to implement an 18-month community-informed maternal death review. The Giving Birth in Nigeria programme was established to find out why pregnant women were dying in communities and to pilot a community accountability mechanism for maternal deaths. This programme was supported by funding from MSD, through MSD for Mothers, the company’s $500 million initiative to help create a world where no woman dies giving life. MSD for Mothers is an initiative of Merck & Co., Inc., Kenilworth, NJ, U.S.A. The programme called for a bottom-up approach to address the challenge of maternal mortality, starting from community led action, pushing for greater collaboration among stakeholders across all levels of decision making and building in sustainable and actionable solutions, for lasting change.
The community review was carried out from May 2019 to May 2020 in six selected states and the FCT, with one state in each geopolitical zone; Bauchi, Bayelsa, Ebonyi, Kebbi, Lagos and Niger State and the Federal Capital Territory. In the year of review, 133 maternal deaths were documented in 18 communities in the six states. Out of these maternal deaths, 52 women died at home, 28 women died in the home of a Traditional Birth Attendant (TBA), 18 deaths occurred in a faith-based institution, and 17 deaths were in a health facility.
Overview of the “Why Are Women Dying’ Report
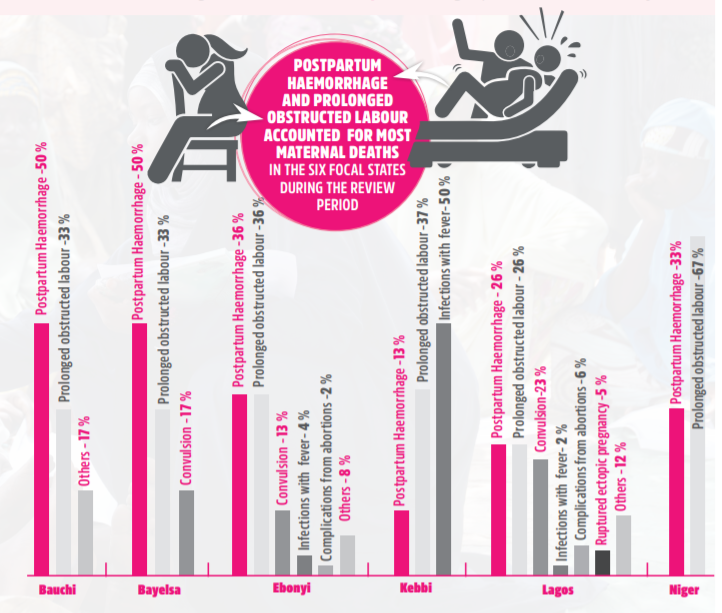
The ‘Why Are Women Dying While Giving Birth in Nigeria?’ report presents a state-by-state analysis of the causes of maternal deaths of women in the communities surveyed. Insights include the health-seeking behaviour of women in communities, why maternal deaths occurred, where women died while giving birth and who attended to them. The report also provides insights into the underlying sociocultural and socioeconomic determinants of maternal health outcomes in these states. It captures the causes, both clinical and underlying, of maternal deaths in communities in Nigeria.
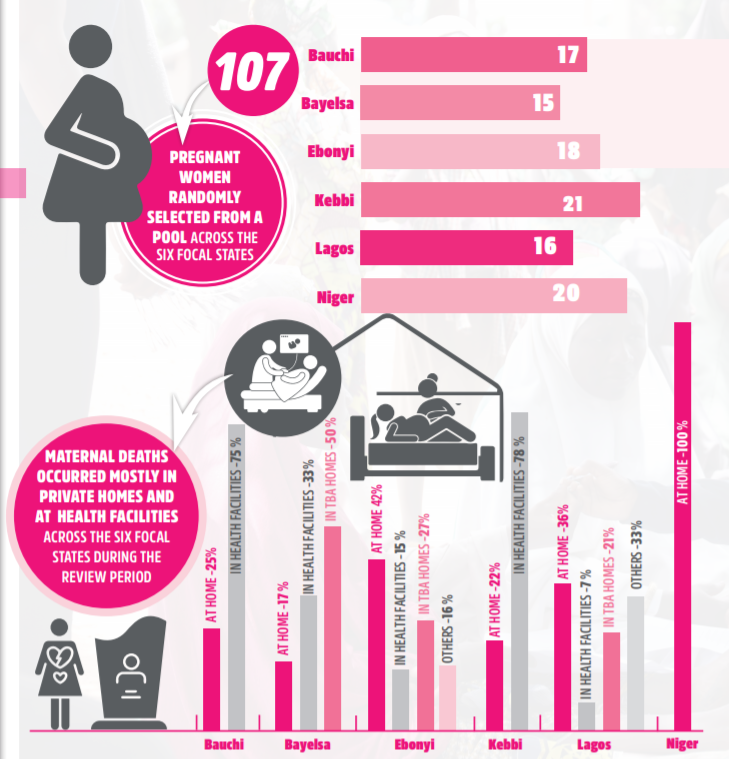
In Bayelsa State, women in local communities have difficulty accessing quality maternal health care because of the riverine terrain in the state. Many have to resort to giving birth with the assistance of traditional birth attendants, locally known as ‘Massagers’. In Ebonyi State, women hold on to the belief that giving birth at home is the only way to show that you are a strong woman, and giving birth in a health facility is a sign of weakness, so births at home with no one present is a continued practice. In Lagos State, giving birth in faith-based centres was widely practiced because of the influence of religious beliefs on maternal health-seeking behaviour. These are a few of the insights presented in the report.
Disseminating Key Findings from the Report
On Monday, 30 November 2020, the consortium comprising of Africare, Nigeria Health Watch and EpiAFRIC, organized a webinar to launch the report, sharing insights, findings and recommendations from the year-long community review of maternal deaths. Critical stakeholders from government, healthcare, academia, civil society and business were present at the dissemination meeting.
Keynote Speaker, Her Excellency Dr. Zainab Shinkafi-Bagudu spoke on the importance of political will in driving better quality maternal health care in Nigeria. She drew from current examples of poor maternal health care delivery in local communities and highlighted the role of political commitment and public-private collaboration to steer better maternal health care for women in communities. “The focus, for reducing maternal deaths in local communities, is to use health education and targeted advocacy to improve health seeking behavior in rural households,” she said, adding, “encouraging community ownership of primary health care using community leaders is key to increasing community demand for better maternal health care”. She said that when there is increased demand for better quality maternal health care, decision makers will be held accountable to supply quality care for women.
Dr. Samuel Oyeniyi, Deputy Director, Safe Motherhood and National Desk Officer, MPDSR, Federal Ministry of Health, spoke on the role of the federal government in establishing structures for the facilitation of better maternal health care in Nigeria. In collaboration with the Rotary Club, the federal government established a platform to collate data to track maternal deaths in Nigeria, called the Nigeria Obstetric Quality Assurance Electronic platform. According to Dr. Oyeniyi, a partnership exists between state governments and LGAs in Nigeria to improve maternal health outcomes at the community level. This partnership is being facilitated through a coordination platform, Reproductive, Maternal, New-born, Child, Adolescent Health (RMNCAH) and has been created to oversee the coordination of tailored solutions to reduce maternal, newborn and childhood deaths in Nigeria. “The MPDSR legislation is at the National Assembly and has gone through the second reading and will soon be passed. It will enhance comprehensive reporting of maternal deaths, protect health care workers and will be positioned to track and account for all maternal deaths in Nigeria,” Dr. Oyeniyi said.
The role of unskilled birth attendants in facilitating maternal health care in communities was a central topic at the virtual meeting. A panel of speakers that included Dr. Daniel Umezuruike, Honourable Commissioner for Health, Ebonyi State, Hajiya Hannatu Abubakar, Maternal and Child Health Coordinator, Bauchi State Primary Health Care Development Agency and Alhaji Moruf Hassan, Coordinator, Association of Traditional Birth Attendants, Epe, Lagos State, discussed how the unskilled workforce in Nigeria can be strengthened to improve the quality of maternal health care.
Dr. Umezuruike noted that comprehensive health insurance and primary health care must be strengthened to improve access to skilled maternal health care at the community level, and to ensure this, state governments must focus on restoring and equipping primary health care centres. Hajiya Abubakar mentioned that a vast array of opportunities to improve maternal health outcomes in communities lies in the hands of traditional birth attendants (TBAs). “Traditional birth attendants who are trained can help identify emergency warning signs during pregnancy and labour. They can also be useful for health education and community sensitisation as they are usually highly respected members of the community” she said.
Alhaji Moruf Hassan said that traditional birth attendants operating in Lagos State are registered and trained for six weeks before they can practice. He added that Lagos State is upskilling and certifying unskilled birth attendants so that they know their limits, can recognize danger signs and are able to refer women to primary health care centres when needed. This is an essential recommendation for other states to adopt in their bid to improve maternal outcomes.
How Do We Stop Women from Dying While Giving Birth in Nigeria?
The ‘Why Are Women Dying While Giving Birth in Nigeria?’ report does not only present causes of maternal deaths in communities in Nigeria, but provides evidence to inform policy and offers recommendations for policymakers, key decision makers and other critical stakeholders to adopt in the drive to end the large number of maternal deaths in Nigeria.
The primary recommendation from the report is the establishment of community Maternal and Perinatal Death Surveillance and Response (MPDSR), through community leadership and state-government-local government-community collaboration. The death of every woman must be counted and investigated, and insights from her death recorded to inform policy and regulations so that solutions are found, so that no woman dies from similar causes. Other recommendations include the enforcement of guidelines and regulations for the operation of unskilled birth attendants. Discussions during the panel discussions highlighted the divergent views and somewhat incoherent strategy that currently exists in Nigeria, when considering the role of TBAs in the continuum of care for pregnant women.

Revitalizing primary health care for better quality maternal health care is critical to ensure that at the point of need, pregnant women have access to quality and affordable healthcare. At present, the level of education of a pregnant women influences her health seeking behavior as well as place of delivery, highlighting the importance of health education. It is important that women have access to a skilled birth attendant able to address any complications that may arise in their pregnancy. During the maternal review, women in communities mentioned a reluctance to visit health facilities because of the often poor attitude of health workers. Ensuring that pregnant women have access to patient-centered care is critical, where the healthcare offered is responsive to her needs and she is treated with dignity and respect.
These findings, insights and recommendations speak to one goal: ending maternal mortality in Nigeria. No woman deserves to lose her life while bringing forth life. It is a fundamental human right of every woman to get better quality health care while giving birth in Nigeria. The ‘Why Are Women Dying While Giving Birth in Nigeria?’ report should be a guide for the establishment of sustainable structures to track maternal deaths of women in communities, derive learning and create sustainable solutions so that no woman dies while giving birth in Nigeria. It starts with each one of us, our religious leaders, traditional rulers, women leaders, men, health care workers, civil society, academia and the government. Together, we need to create a Nigeria where all mothers lives matter, especially women in communities.
The ‘Why Are Women Dying While Giving Birth in Nigeria?’ report was launched on Monday, 30 November 2020. Follow this link to view or to download.



Thank you for this beautify report highlighting the need to account for the death of every woman giving life. But in all of this report, the role of the cost of accessing services was missing. Many people don’t just prefer to go to faith homes or TBAs, they do so to save cost as birth at the faith homes/TBAs is believed to be cheaper than at the facility.