By Lydia Atieno (Lead Writer)
Thirty-five-year-old Christelle Uwamahoro had always been aware of the significance of cervical cancer screenings. Community health workers in her village went door to door, educating residents and emphasising the importance of early screening for cervical cancer. “Despite this knowledge; I had second thoughts about screening,” she said. However, this all changed when a friend of hers was diagnosed with advanced cervical cancer.
Shaken by this information, Uwamahoro decided to get screened. This singular action saved her life as she was diagnosed of early-stage cervical cancer. Cervical cancer is the most treatable type of cancer if detected early and managed effectively. As a result of her cancer being diagnosed early and managed properly, she is now cancer free.
Cancer control strategies
Cervical cancer is the fourth most common cancer among women globally, and the most common cancer among Rwandan women. According to World Health Organization (WHO) data, cervical cancer accounted for 940 of the total deaths in Rwanda in 2019. Since 2011, the country has implemented vaccination, screening, and treatment strategies to control cervical cancer beginning with the National Vaccination Programme against Human Papillomavirus (HPV) — the first African country to do so.
The HPV vaccine programme began in schools, targeting girls aged 12 to 15. It was also made available at health facilities for a limited period for 12-year-old girls who were out of school or who were absent during vaccination days. The HPV vaccine was later incorporated into the country’s immunisation programme and healthcare system.
According to Francois Uwinkindi, Director of Non-communicable Diseases at Rwanda Biomedical Center, the HPV vaccine is administered in two doses, with a follow-up vaccine in six to 12 months after the initial vaccination. “Immunisation is provided to all girls between the ages of 11 and 15. In addition to being offered at schools, the HPV vaccine is also available at health centers nationwide,” he added. Two years after the programme began, it had achieved over 90 percent coverage and has maintained that level.
The ‘screen and treat’ programme
Following the success of the vaccination programme, a low-cost cervical cancer screening programme was implemented. The government piloted a ‘screen-and-treat’ programme across seven hospitals and 89 health centers in five districts that ended in July 2021. The goal was to screen for HPV at least 70% of women between the ages of 30 and 49 living in the targeted districts.
Community health workers were deployed in every community to raise awareness and provide information about cervical cancer and the importance of early detection. The aim of the community outreach was to encourage women to access the screening services, which are currently available in 29 hospitals (district, provincial, and referral) and 249 health centres across the country. “The screening reach is at 23 percent and the country has the plan to reach 70 percent by 2027,” said Dr Uwinkindi. Women are screened using one of three methods: HPV DNA testing, Visual Inspection with Acetic acid (VIA), or Pap Smear.

According to Dr Theodomir Sebazungu, a gynecologist at the Muhima Health Center in Kigali, the results take about 10 days to process, and if the patient tests positive for HPV, they are contacted by phone or through a community health worker, who then communicates with the patient to return for further treatment. Precancerous cervical lesions can be managed at the health centre by nurses and midwives. Cancer cases that have been confirmed are referred to district or referral hospitals for further investigations, diagnosis, and treatment which may include surgery, radiotherapy and chemotherapy.
Prohibitive cost of treatment
Cancer treatment is prohibitively expensive. A single dose of HPV vaccine costs $268.773 while an HPV test costs $25. Recognising that the cost of vaccination, screening and treatment services, is a barrier to their uptake, the Ministry of Health, in collaboration with Rwanda Biomedical Centre (RBC) funds these interventions with support from partners like, Unitaid, Partners in Health and the World Bank.
The screening programme has been added to Rwanda’s community health insurance plan, Mutuelle de santé, the country’s largest health insurance scheme, which covers the healthcare needs of 88% of Rwanda’s 12 million people. For women of eligible age, the cost of screening is $3 per person under insurance. The community health insurance also covers all cervical cancer treatment for the poorest people (surgery, radiotherapy and chemotherapy), but only surgery and radiotherapy for the rest of the population. However, chemotherapy for this category of patients is covered by partners.
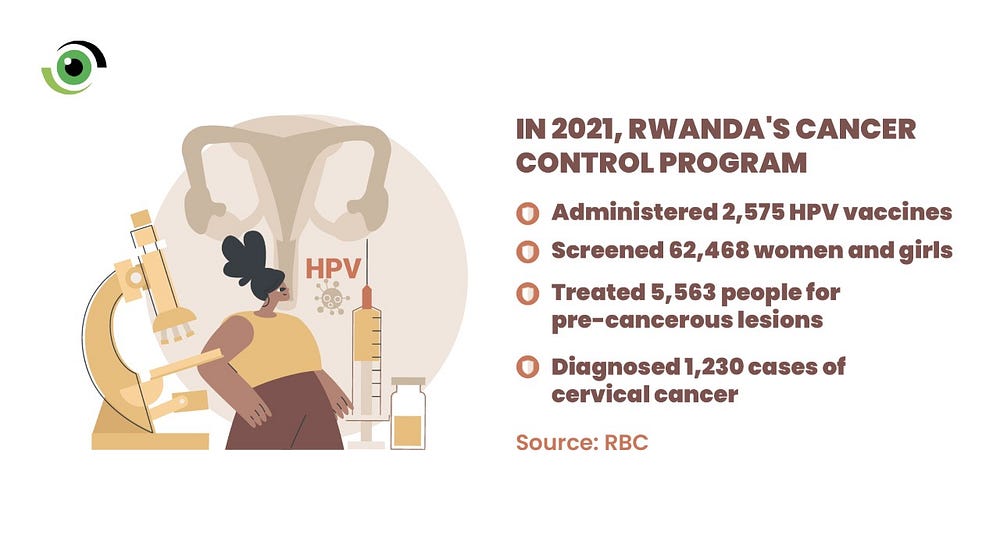
Recent data from RBC indicates that in 2021, 2,575 HPV vaccines were administered, 62,468 women and girls screened, 5,563 people treated for pre-cancerous lesions and 1230 cases of cervical cancer diagnosed. With increased awareness of screening and a successful HPV vaccination programme for 12-year-old girls, Dr Uwinkindi believes the country is on track to eliminate cervical cancer.
Towards cancer elimination
According to the WHO Global strategy to accelerate the elimination of cervical cancer as a public health problem, to eliminate cervical cancer, countries must reach and maintain an incidence rate of below four per 100,000 women. In 2020, Rwanda’s incidence rate was 28.2, and while the country has made some notable progress in cervical cancer control in recent years, more work is needed to increase coverage for screened women, as they are sometimes lost in follow up.
Cervical cancer elimination is expensive and although RBC in collaboration with partners has been able to make screening free for the population, Dr Fidel Rubagumya, a Clinical and Radiation Oncologist at Rwanda Military Hospital says the HPV/DNA tests recommended by the WHO, due to their high sensitivity and specificity are not affordable. He revealed that the low-cost methods available in Rwanda are not specific and can occasionally detect false positives.
Other issues identified in the Rwanda National Cancer Control Plan (NCCP) 2020 to 2024 are lack of community knowledge about cancer signs and symptoms, a lack of decentralisation as hospitals with the capacity to diagnose and treat cancer are still not equitably located throughout the country, the high cost of treatment, particularly when personal costs are incurred during the course of treatment and the lack of comprehensive services.
The overarching goal of the NCCP is to leverage past experiences in order to reduce mortality from common curable cancers and to ensure that prioritised diagnosis and treatment services are provided in an integrated, equitable, and sustainable way, particularly at the primary care level. However, without adequate funding, this plan is not sustainable. As a result, encouraging investment through Public Private Partnership (PPP) financing models, increasing domestic financing of cancer prevention and control interventions, and developing innovative financing models for cancer control interventions is a commendable course of action.
Cervical Cancer Awareness
Cervical Cancer Awareness Month is observed in January. A fantastic opportunity to raise awareness about cervical cancer and HPV vaccination, as well as to join the advocacy to eradicate cervical cancer within a few generations.
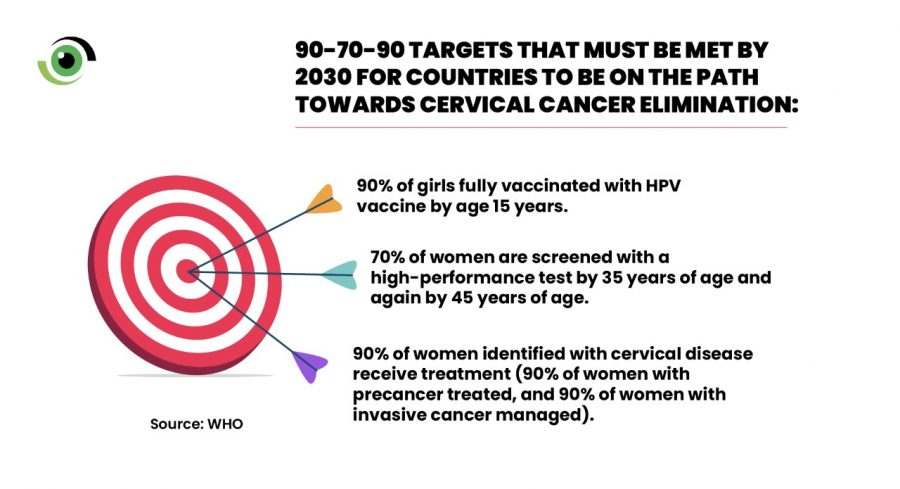
Infection with high-risk human papillomavirus (HPV), and extremely common virus transmitted through sexual contact is linked to 95% of all cervical cancer cases. As a result, during this cervical cancer awareness month, advocacy must be targeted towards ensuring that global efforts are intensified to guarantee a world where cervical cancer is eliminated as a public health problem, following the 90–70–90 targets that must be met by 2030 for countries to be on the path towards cervical cancer elimination:
· 90% of girls fully vaccinated with HPV vaccine by age 15 years.
· 70% of women are screened with a high-performance test by 35 years of age and again by 45 years of age
· 90% of women identified with cervical disease receive treatment (90% of women with precancer treated, and 90% of women with invasive cancer managed).
Individuals must also endeavour to,
. Get informed: Find out the facts about cervical cancer and the human papilloma virus (HPV) that causes it. Help educate other women in your life too.
. Get screened: Cervical cancer screening typically starts at age 30 and is repeated periodically.
.Get vaccinated: The HPV vaccine is given in 2 doses that should begin when a girl is between 9 and 14 years old.


