After six months of anxiety, panic and unrest as a result of the COVID-19 pandemic, medical doctors at the University of Port Harcourt Teaching Hospital (UPTH) have treated and discharged the last patient in the hospital’s isolation centre.
Records from the Nigeria Centre for Disease Control, as at the time of publication, show that Rivers State has a total number of 2,735 confirmed cases of COVID-19 with 2,602 already discharged, 59 deaths and 74 persons on admission.
Dr Datonye Alasia Dennis, Head of the Respiratory and Infectious Disease Unit at UPTH, said that at the advent of the COVID-19 pandemic, seeing the impact on other countries, his team re-strategized and prepared to fight the pandemic, although “it was not as easy as it seems”, he said.
When the pandemic hit, the hospital decided to expand its facilities. The Accident and Emergency Response facility which used to be a two or three-bed holding area, was expanded to hold close to 20 beds. The intensive care unit for dealing with severe infectious disease cases was also increased to be able to care for a minimum of six patients.

“There was increased awareness and training for staff on infectious disease knowledge and response”, Dr Alasia said, adding that there were a lot of people within the hospital who had the capacity and skills to offer in infectious disease response, such as cleaners, attendants and epidemiologists, who prior to the pandemic had not had the opportunity to put these skills to use. “All they needed was some training and they brought out their skills to fight the virus,” he said.
Fighting COVID-19
In fighting infectious diseases, hospitals create red and green zones to demarcate areas where personal protective equipment (PPE) must be worn. Whenever doctors leave the green zone to the red zone, they ensure they put on the full PPE required to protect themselves from contracting the virus.
Dr Alasia pointed out that, “Once we are done with the COVID-19 patients inside the red zone, we go through a pathway where the full protection kits will be dropped. Those things that are infectious will all be taken off and decontaminated with chlorinated water, and once we get home, we bathe again and ensure our clothes are taken off”, adding, “Our families are used to not touching us once we return from work”.

Outside the green zone, there are handwashing facilities with two taps; one with chlorinated water, and the other with normal water to wash after disinfecting your hands.
Professor Kingsley Stanley, Chairman, Medical Advisory Committee (CMAC) recalls that during the peak of the coronavirus, the hospital’s management, headed by Professor Henry Ugboma, set up a 20-bed isolation centre, and later on added 10 beds to make it 30, although, that did not solve the surge.
“We had to open another centre near the accident and emergency wards which has 25 bed spaces. By the time we finished, we noticed the curve had flattened. As we speak, we do not have any single patient at the centre,” Prof. Stanley said.
Ensuring safe maternal health during the COVID-19 pandemic
The UPTH leadership put in place a multidisciplinary team of 10 members who were tasked with caring for pregnant COVID-19 patients until they gave birth. The team is made up of two anaesthetics, two obstetrician-gynaecologists, one paediatrician, theatre nurses, a midwife and an infection and prevention control specialist.

Dr. Alasia said the hospital successfully treated five COVID-19 pregnant women. Amongst the five women, two were successfully gave birth through caesarean sections, another through vaginal delivery, and the two others were treated for COVID-19 and were able to return home until it was time for them to give birth. “One of them came and delivered her baby and the other is yet to deliver”, Alasia said.
Dr Omosovie Maduka doubles as the UPTH head of community medicine and facility manager of the COVID-19 treatment centre. She said from the beginning of admission of the pregnant COVID-19 patients, while the women were still suspected to be positive, and samples had been collected, the women were kept separate from other pregnant women in the antenatal and labour wards to avoid transmission. “When the results came out and we confirmed that they were positive, they were moved to the isolation centre. Before the Caesarean section, these women were still in the isolation centre and when they delivered, they were moved to the treatment centre,” she said.
The hospital also put in place triage areas. Pregnant women who come for antenatal and delivery were asked basic questions relating to COVID-19, and if suspicions were raised, “a team in the Obstetric-Gynaecology centre that is permanently stationed and specifically trained to manage suspected and confirmed cases of COVID-19 will be called in to do a second assessment and if they agreed with the second assessment, a sample will be collected for testing and the management and treatment comes on board if the person is positive”, Maduka added.
If the pregnant woman does not present with any symptoms related to COVID-19, she is allowed to see the doctor in line with COVID-19 preventive measures. Omosivie said there is a “no mask, no entry” policy that is enforced for both staff and patients at the hospital.
Delivery of COVID-19 infected pregnant women requires extra precautions to prevent exposure to the coronavirus. “For COVID-19 pregnant women, we have to go higher in terms of infection prevention and control practice. We have to put on a full hazard suit, wear a headcover with a full n95 facemask, shields, head cover, gloves and of course we have to look at the environmental management to ensure that you deal with respiratory droplets”, Alasia said, adding that the hospital also rearranged the postnatal ward in order to meet physical distancing requirements.

Goodness Uchendu is a nursing mother who gave birth at the hospital during the peak of the COVID-19 outbreak. She said she was tense knowing that the hospital was handling COVID-19 patients, but with the directives of the management to observe preventive measures, she wore her face mask and observed physical distancing during her antenatal visits. “In the labour room, I can remember we had two beds, and we were made to wear our masks even after successful delivery”, said Uchendu. In the Immunisation hall, there are stickers reminding patients of COVID-19 preventive measures and a veronica bucket filled with water and soap kept for nursing mothers to wash their hands before taking a seat.
Sustaining immunisation gains in the midst of a pandemic
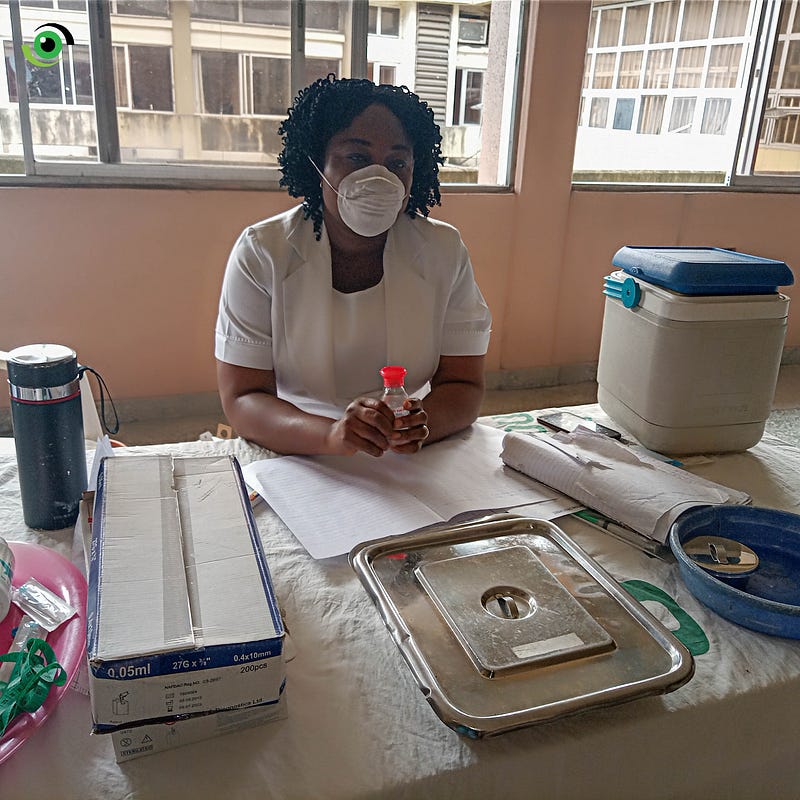
Uche Okoro is the Chief Matron at the UPTH Immunisation Centre. She said that before each baby is immunised, she and other health workers sanitise their hands with highly concentrated alcohol-based sanitisers, and at the end of the day, they wash their hands with soap and water before going home. If mothers bring their babies for immunisation without wearing a mask, instead of sending them back home, “We improvise. We ask them to use their handkerchief to cover their nose because many of them come from afar”, Okoro said.

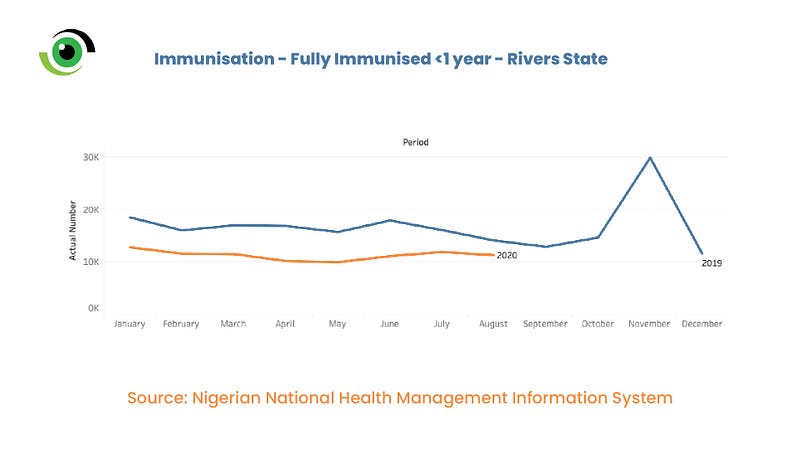
When the COVID-19 pandemic hit Nigeria, many mothers stopped bringing their babies for immunisation out of fear of their children contracting the virus. Data from the Federal Ministry of Health shows that due to the COVID-19 pandemic, the rate at which mothers brought their babies for immunisation drastically reduced. Data from the Nigerian National Health Management Information System showed that in Rivers State, in May 2019, 15,667 children below the age of 1 had been immunised while in the same month in 2020, only 9,904 children below the age of 1 had been immunised in May 2020. Before COVID-19, the hospital’s immunisation hall was always full. The Deputy Matron, Helen Eze thought it was a result of the lockdown as many postnatal mothers come from afar.
Deputy Matron Eze said she picked up her phone and started calling the nursing mothers based on the numbers provided on the immunisation registry to find out why they suddenly stopped coming for routine immunisation. “Many said UPTH has COVID-19 while some promised to come for immunisation”, Eze said.
The challenge of keeping the doors open in the midst of a pandemic
One challenge the team of doctors fighting COVID-19 faced was having patients who had severe illness and difficulties in breathing present late, usually coming to the hospital at the point of death. Dr Alasia said that the majority of deaths recorded were of patients who came late, even though the doctors tried their best to ensure that they survived.
According to Dr Alasia, none of the team members fighting COVID-19 died, but two other health workers in the hospital contracted the disease and died. He said it was difficult to pinpoint how they contracted the virus. Prof. Stanley stated that the hospital management had put in measures to ensure that health workers and patients are safe from COVID-19, despite the enormous challenge the hospital faces which includes funding.
He said hospital funds were exhausted in the fight against the virus as every patient treated for COVID-19 was treated for free, “including the food the patients ate during their stay in the hospital. This was all freely provided by the hospital”. He noted that the hospital had to rely on already declining internally generated revenue, which later dried up when there was a restriction placed on movement and no one was coming to the hospital, except for the COVID-19 patients.
Another challenge was discrimination. Health workers fighting infectious diseases globally have faced discrimination. UPTH health workers at the isolation centre are no exception. Some staff working at the UPTH COVID-19 isolation centre said they experienced stigmatisation from their colleagues working in UPTH. “Even when we enter a taxi from the Hospital, some of our staff who knew us as people working in the isolation centre avoid us, they even go as far as alighting from the vehicle before their destination”, said one of the health workers working at the UPTH isolation centre who asked for their name not to be mentioned. The stigmatisation of health workers was borne out of fear, but Prof. Stanley said the hospital management began to sensitise the staff and as a result stigmatisation has reduced.

Looking Ahead
The work done by doctors and UPTH management, despite the limited funding and other challenges faced will remain important as every health worker will be more safety conscious to avoid the rapid increase of COVID-19. One lesson these doctors learnt is the importance of collaboration to save mothers and their babies amidst the pandemic.
It is important for the hospital to continue sensitising post-natal mothers to bring their babies for immunisation, despite the pandemic to sustain immunisation gains and protect their children from vaccine preventable diseases.
Health workers fighting infectious diseases like COVID-19 should continue to be supported to do their work well, without stigmatisation. Many go the extra mile to save lives, and some have lost their lives in the fight. The requisite funding that is necessary to ensure they are able to work must be provided so that they can continue to provide care to mothers and their babies. They can’t do this alone.
How has the teaching hospital in your state managed to provide services in the midst of the COVID-19 pandemic? Drop a comment below or drop us a line on social media, @nighealthwatch on Twitter or @nigeriahealthwatch on Facebook and Instagram!


